Colds and flu are both highly contagious and, in the initial stages, a bad cold and a mild case of the flu might seem alike. Unlike a cold, though, the flu is a serious illness that can have life-threatening complications. Here is a comparison of cold and flu symptoms.
This information was adapted from the U.S. Centers for Disease Control and Prevention (CDC) website.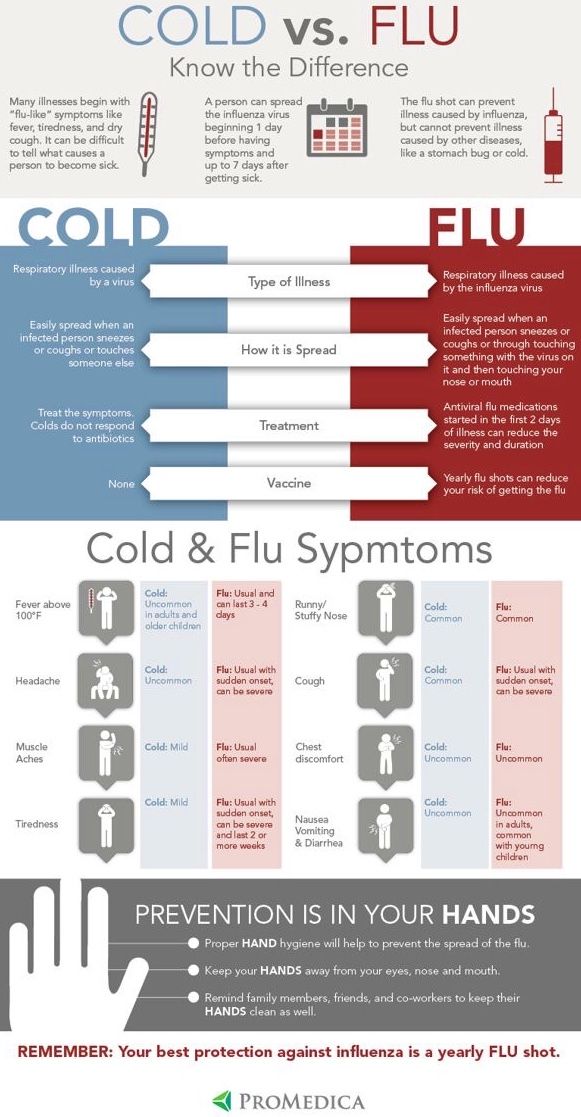 For more information, visit the CDC's flu page.
For more information, visit the CDC's flu page.
UCSF Health medical specialists have reviewed this information. It is for educational purposes only and is not intended to replace the advice of your doctor or other health care provider. We encourage you to discuss any questions or concerns you may have with your provider.
Can You Tell If It’s the Flu or COVID-19?
UCSF experts help explain the differences between flu and COVID-19, when to get a test, and why you shouldn’t try to diagnose yourself.
Facts About the Flu
Find facts about influenza, aka "the flu," including, prevention, signs and symptoms, transmission, diagnosis, treatment and complications. Learn more here.
When to Call Your Doctor About the Flu
If you are at special risk of flu complications, contact your doctor as soon as your symptoms begin. Learn more here.
Center for Geriatric Care
3575 Geary Blvd. , First Floor
, First Floor
San Francisco, CA 94118
(415) 353-4900
M-F, 8:30 a.m. - 5 p.m.
Family Medicine Center at Lakeshore
1569 Sloat Blvd., Suite 333
San Francisco, CA 94132
(415) 353-9339
M-F, 8 a.m. - 5 p.m.
General Internal Medicine at Post Street
1545 Divisadero St., First and Second Floors
San Francisco, CA 94115
(415) 353-7900
M-F, 8:30 a.m. - 5 p.m.
General Internal Medicine at Sutter Street
1701 Divisadero St., Suite 500
San Francisco, CA 94115
(415) 353-7999
M-F, 8 a.m. - 5 p.m.
Primary Care at China Basin
185 Berry St., Lobby 1, Suite 1000
San Francisco, CA 94107
(415) 514-4533
Primary Care at Laurel Village
3490 California St., Suite 200
San Francisco, CA 94118
(415) 514-6200
M-F, 8 a.m. - noon, 1 - 5 p.m.
Women's Health Primary Care Clinic
2356 Sutter St., Third and Fourth Floors
San Francisco, CA 94143
(415) 885-7788
M-F, 8 a.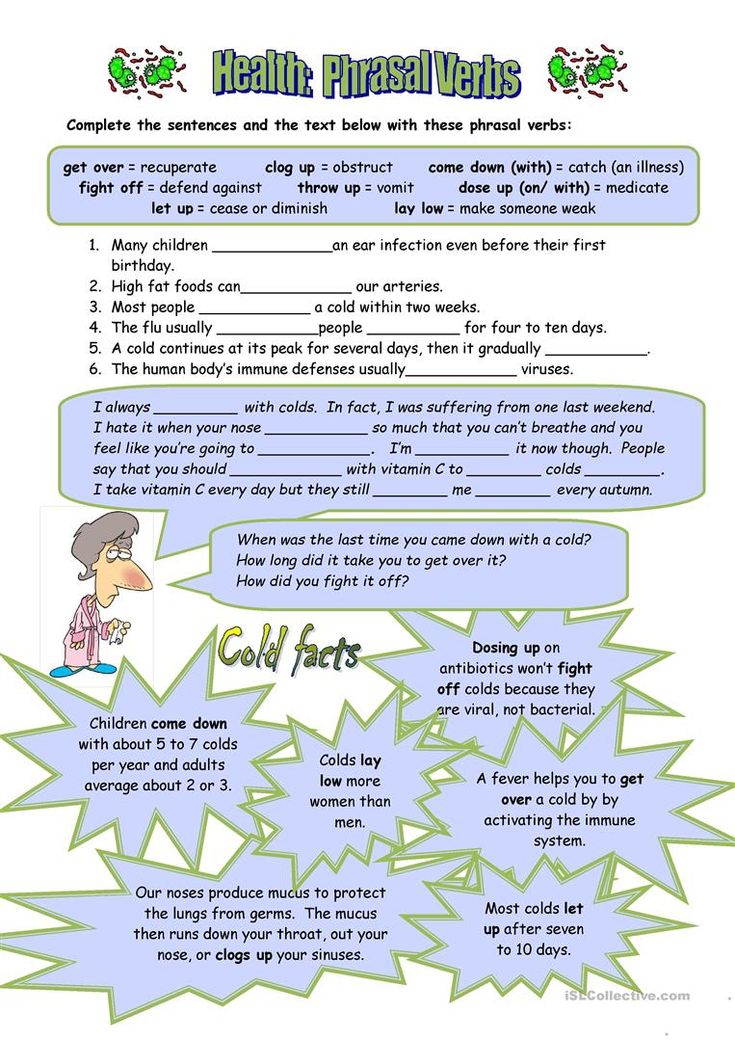 m. - 5 p.m.
m. - 5 p.m.
The flu is caused by a virus. Viruses are generally passed from person to person through the air when an infected person sneezes or coughs.
But the virus can also live for a short time on objects like doorknobs, pens, pencils, keyboards, phones, and cups or eating utensils. So you can also get the flu by touching something that has been recently handled by someone infected with the virus and then touching your own mouth, nose, or eyes.
Each person may experience symptoms differently. The flu is called a respiratory disease, but it can affect your entire body. People usually become very sick with several, or all, of the following symptoms:
Cough, often becoming severe
Extreme exhaustion
Fatigue for several weeks
Headache
High fever
Runny or stuffy nose
Severe aches and pains
Sneezing at times
Sometimes a sore throat
Vomiting and diarrhea
Fever and body aches usually last for 3 to 5 days, but cough and fatigue may last for 2 weeks or more.
The symptoms of the flu may look like other medical problems. Always talk your healthcare provider for a diagnosis.
The flu is diagnosed based on your symptoms. Lab tests may be used to confirm the diagnosis, if necessary.
Specific treatment for the flu will be determined by your healthcare provider based on:
Your age, overall health, and medical history
Extent and type of flu, and severity of symptoms
How long you’ve had symptoms
Your tolerance for specific medicines, procedures, or therapies
Expectations for the course of the disease
Your opinion or preference
The goal of treatment for the flu is to help prevent or decrease the severity of symptoms. Treatment may include:
Antiviral medicines. They can reduce how long you’ll have the flu, but they can’t cure it. They have to be started within the first 2 days of the illness. These medicines do have some side effects, such as nervousness, lightheadedness, or nausea. These medicines are prescribed by a doctor.
They can reduce how long you’ll have the flu, but they can’t cure it. They have to be started within the first 2 days of the illness. These medicines do have some side effects, such as nervousness, lightheadedness, or nausea. These medicines are prescribed by a doctor.
Medicines. There are medicines for congestion and nasal discharge. You can also take medicine to relieve aches and fever. Do not give aspirin to children with fever. The drug of choice for children is acetaminophen.
Rest. Bed rest and increased intake of fluids.
Talk with your healthcare provider for more information.
The most common complication of the flu is pneumonia. It can also cause serious muscle and central nervous system complications. Of those who get the flu, between 3,000 and 49,000 will die from it or from complications. Most of these deaths happen in people ages 65 and older.
Most of these deaths happen in people ages 65 and older.
A new flu vaccine is made each fall. Everyone ages 6 months and older should get a flu shot each year. It is usually recommended for specific groups of people, as well as for anyone who wants to avoid having the flu.
The flu shot is safe. The CDC and the FDA closely watch vaccine safety. Hundreds of millions of flu vaccines have been safely given across the country for decades.
The flu shot can’t give you the flu. The most common side effects from a flu shot are:
If you have them at all, these side effects are usually mild and last a short time.
The effectiveness of the vaccine varies from one person to another. It can depend on factors such as age and overall health.
The following may also be helpful for preventing the flu:
When possible, avoid or limit contact with sick people.
Wash your hands frequently to reduce the risk of infection.
Cover your nose and mouth when coughing or sneezing to limit spread of the virus.
The flu causes complications that may develop into a more serious disease or become dangerous to some people. This includes older adults and those with chronic medical problems. Always talk with your healthcare provider to find out if you should receive the flu shot.
Although the flu shot is safe, some people should NOT be vaccinated. These include:
People who are allergic to eggs
People who have had a severe reaction in the past after getting the flu shot
People who are sick with a fever (these people should get vaccinated after they have recovered)
Babies who are age 6 months old or younger
People who have a history of Guillain-Barré syndrome, a severe paralyzing illness, after getting the flu shot
The CDC recommends getting the flu shot every year, as soon as it becomes available in your community.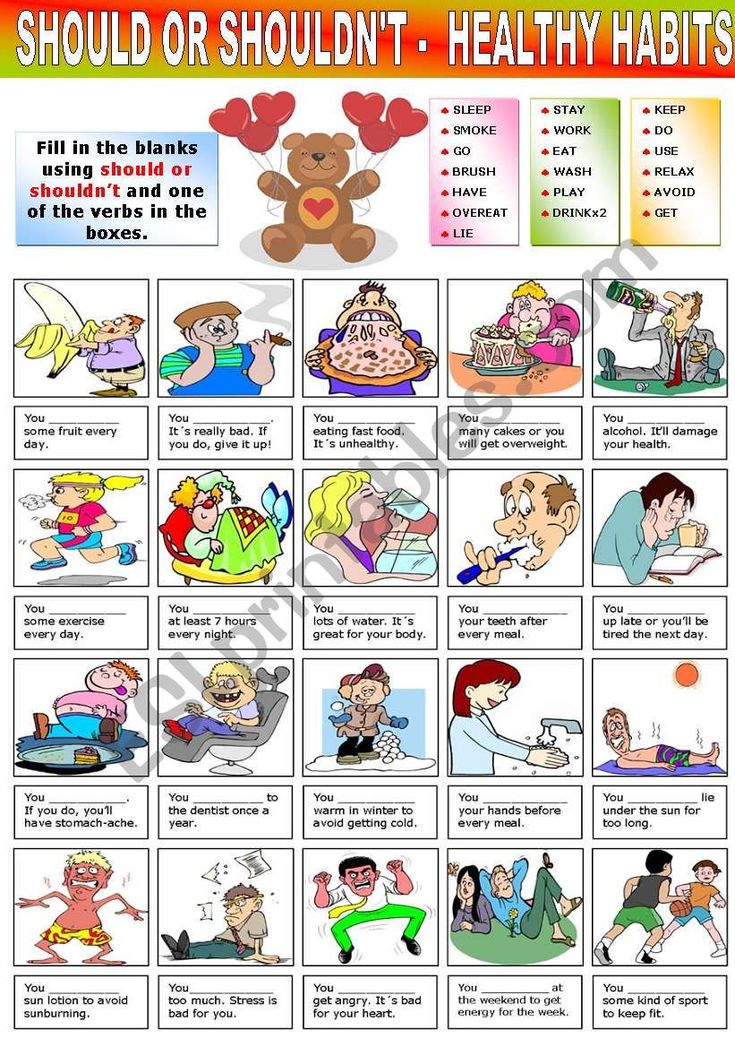 Flu season can begin as early as October and most commonly peaks in the U.S. in January or February, but flu seasons are unpredictable. The flu shot takes 1 to 2 weeks to become effective.
Flu season can begin as early as October and most commonly peaks in the U.S. in January or February, but flu seasons are unpredictable. The flu shot takes 1 to 2 weeks to become effective.
The CDC recommends that travelers have the flu vaccine at least 2 weeks before planned travel to allow time to develop immunity. Talk with your healthcare provider for more information.
For most people, the flu can be treated at home without treatment from your healthcare provider. However, if your condition or situation makes you more susceptible to complications from the flu, tell your healthcare provider when you suspect you have the flu. If your symptoms get worse or you have new symptoms, let your healthcare provider know.
The flu is an easily spread viral respiratory tract infection.
The flu is caused by viruses that are generally passed from person to person through the air.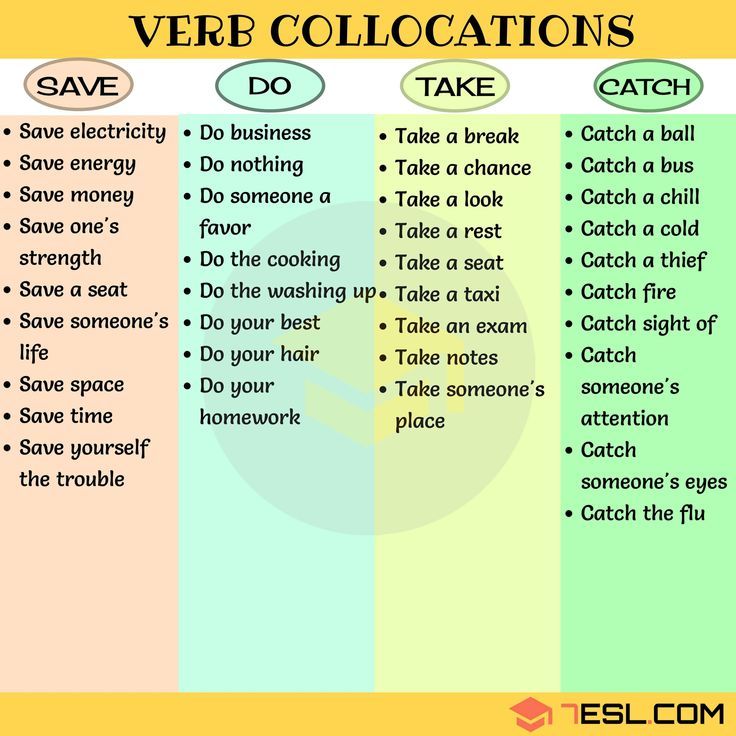
The flu is treated with bedrest, increased fluid intake, and medicines to treat discomfort and fever
Antiviral medicines taken within the first 2 days of illness can reduce the length and severity of the disease but does not cure it.
Getting the flu shot every year is the best prevention.
Almost every person on the planet suffers from 1 to 15 (average 4) episodes of SARS annually. 1 The high incidence is due to the fact that respiratory viruses are numerous, variable and highly contagious. The spread of infections contributes to the neglect of prevention.
At an early stage, patients often do not realize that they can infect healthy people, and do not take protective measures. And after a few days of illness, many are sure that they no longer secrete viruses. In the article, we found out how long a person is contagious with ARVI, and when it is possible to contact others without risk.
In the article, we found out how long a person is contagious with ARVI, and when it is possible to contact others without risk.
SARS is a broad group of viral infections. Despite the different types of pathogens (about 200 types 2 studied), they have similar ways of spreading, development mechanisms and symptoms. All SARS affect the upper respiratory system, and their typical symptoms are runny nose, sneezing, coughing, sore throat and fever.
About half of all ARVI pathogens are rhinoviruses. 2 Influenza, parainfluenza, coronaviruses, adenoviruses, respiratory syncytial viruses are common. Sometimes with ARVI, several pathogens are isolated simultaneously - in these cases, the disease is more severe. 3
As for the incubation period, it depends not only on the properties of the pathogen, but also on the characteristics of the body and the strength of the immune response. Most often, from the moment of infection with SARS to the appearance of the first symptoms, it takes from 2 days to a week. 3 The main danger is that even in the absence of signs of infection, the patient can infect others.
Most often, from the moment of infection with SARS to the appearance of the first symptoms, it takes from 2 days to a week. 3 The main danger is that even in the absence of signs of infection, the patient can infect others.
When the virus enters the body, it attaches to the shell of a healthy cell, penetrates through it and begins to multiply. At the next stage, the daughter virions leave the infected cell and actively spread throughout the body, infecting new cells. This cycle is repeated many times until a sufficiently large number of viruses accumulate in the body. On average, this occurs on the 3rd day after infection. During this period, the patient poses the greatest danger to others, since coughing and sneezing releases the maximum amount of viruses. As a rule, the symptoms of the disease on this day are especially pronounced. 3
A direct-acting antiviral drug - Nobasit - acts immediately after the virus enters the body.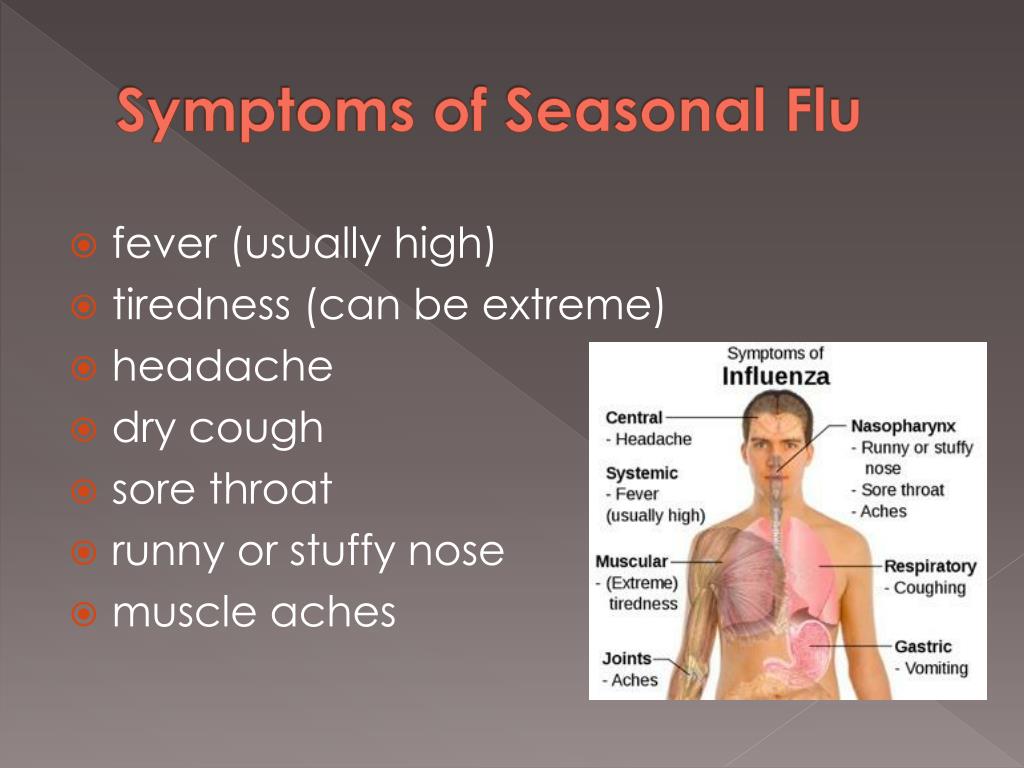 The active substance of the drug prevents the penetration of the virus into cells by blocking the hemagglutinin protein. 4 Doctors recommend starting the drug within the first 48 hours of the onset of the disease to limit the spread of infection throughout the body and prevent infecting others. Thanks to the proven directed action on the cause of acute respiratory viral infections, Nobasit helps to reduce the severity of the main clinical symptoms - cough, runny nose, nasal congestion, etc., and helps to reduce the duration of the disease. 5
The active substance of the drug prevents the penetration of the virus into cells by blocking the hemagglutinin protein. 4 Doctors recommend starting the drug within the first 48 hours of the onset of the disease to limit the spread of infection throughout the body and prevent infecting others. Thanks to the proven directed action on the cause of acute respiratory viral infections, Nobasit helps to reduce the severity of the main clinical symptoms - cough, runny nose, nasal congestion, etc., and helps to reduce the duration of the disease. 5
Active release of viruses into the environment continues for several days. On the 5th day from the onset of the disease, specific antibodies against the pathogen are produced. Shedding of viruses is drastically reduced, and the chance of infecting others is reduced. By this time, the symptoms of SARS are weakening. This happens in most cases, but sometimes a recovered person remains contagious for up to 14 days - until the pathogen is completely removed from the body.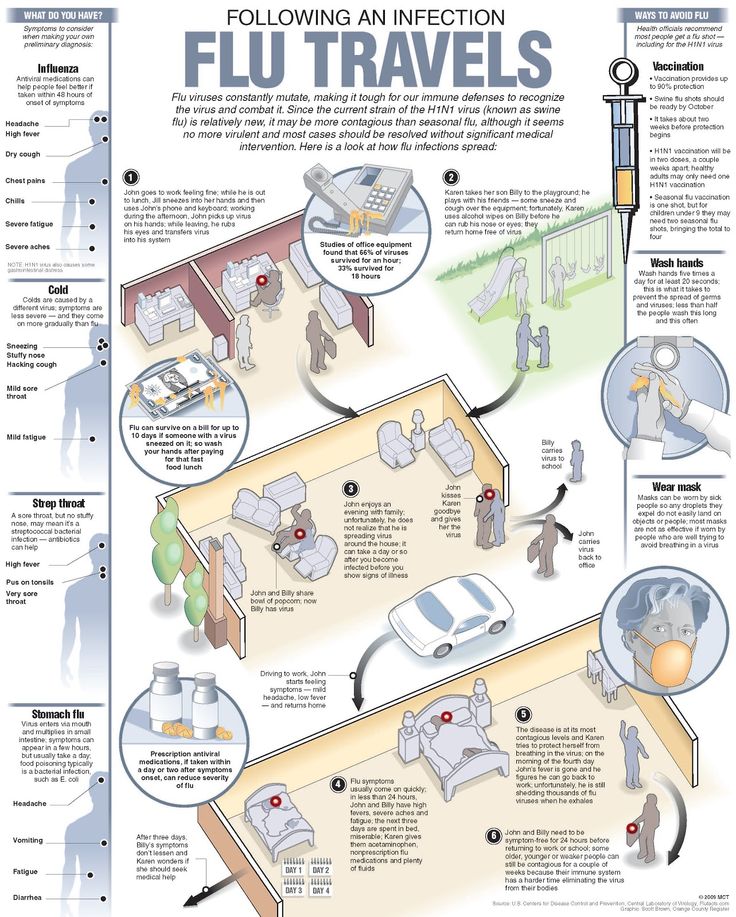 3
3
It can be said that a person stops spreading the infection about two weeks after the onset of the disease and can come into contact with healthy people without risk. Although usually the isolation of viruses stops earlier - with the disappearance of symptoms of SARS.
The main route of transmission of viral infections is airborne. When coughing, sneezing and talking, a sick person releases viruses that are contained in particles of saliva and mucus. Due to their very small size (much smaller than bacteria), ARVI pathogens remain longer in the aerosol and spread over long distances (up to 2–3 m). 6
When the aerosol settles, the droplets dry up and most viruses die. But some of them retain viability and pathogenic properties for a long time. For example, adenoviruses can live outside the human body for up to 14 days. 2 So, in addition to airborne droplets, the airborne transmission route (by inhalation of dust that contains viruses) cannot be ruled out. Adenoviruses and rhinoviruses can also be spread by contact. The pathogen is transmitted through contaminated hands and household items.
Adenoviruses and rhinoviruses can also be spread by contact. The pathogen is transmitted through contaminated hands and household items.
Given the methods of transmission of diseases, during periods of seasonal outbreaks of incidence (for most SARS this is autumn, and for influenza - winter), precautions should be taken.
● Try to reduce the use of public transport and, if possible, avoid crowded places.
● When outdoors, do not touch your face with your hands.
● Wash your hands frequently or treat them with antiseptic solutions.
● At home, regularly carry out wet cleaning, ventilate the rooms.
● Dress for the weather, don't overcool.
● If someone in the family is already sick, give him a separate room, individual dishes, limit contact with him.
● Try to lead a healthy lifestyle, eat well and consume enough vitamins - this will help maintain a strong immune system.
➢ More than 200 ARVI pathogens are known. Respiratory infections caused by different viruses have common features and differences, but the incubation period depends not only on the properties of the pathogen, but also on the characteristics of the body and the strength of the immune response.
Respiratory infections caused by different viruses have common features and differences, but the incubation period depends not only on the properties of the pathogen, but also on the characteristics of the body and the strength of the immune response.
➢ Especially dangerous are contacts with a sick person in the first 3 days after infection - it is during this period that symptoms usually appear most clearly.
➢ As symptoms improve, the risk of infection decreases, but finally disappears only after 2 weeks from the onset of the disease.
➢ In order not to get infected during colds, try not to touch your face on the street, wash your hands more often, dress according to the weather and lead a healthy lifestyle.
1 Kovtun TA, Tutel'yan AV, Shabalina SV Modern ideas about the epidemiology and etiology of acute respiratory diseases of the respiratory tract in children // Epidemiology and vaccine prevention. - 2010. - No. 5.
2 Larina V. N. et al. Acute respiratory viral infections and influenza: etiology, diagnosis and treatment algorithm. - RMJ. Medical review. - 09/11/2019. - No. 9 (1).
N. et al. Acute respiratory viral infections and influenza: etiology, diagnosis and treatment algorithm. - RMJ. Medical review. - 09/11/2019. - No. 9 (1).
3 Belan EB, Sadchikova TL Acute respiratory viral infections: current view on the problem and modern approach to treatment // BC. Medical review. — 12/25/2018. - No. 11.
4 Instructions for medical use (Nobasit®, film-coated tablets 250 mg; RU: LP-003508 of 03/16/2016)
5 Lioznov D.A., Karnaukhova E.Yu., Zubkova T.G., Shakhlanskaya E.V., Evaluation of the effectiveness of the ARVI treatment regimen, including etiotropic (enisamia iodide) and symptomatic therapy // Therapeutic archive No. 3 - 2020
6 Pozdnyakova MG, Shelekhova SE, Erofeeva MK Epidemiology of SARS and the possibility of their prevention // Portal Eurolab.
About the product Download manual
WHO/T. Pietrasik
Pietrasik
© A photo
Seasonal influenza is an acute respiratory infection caused by influenza viruses that circulate throughout the world.
There are 4 types of seasonal influenza viruses - types A, B, C and D. Influenza A and B viruses circulate and cause seasonal epidemics diseases.
Influenza A viruses are subdivided into subtypes according to combinations of hemagglutinin (HA) and neuraminidase (NA), proteins on the surface of the virus. Viruses are currently circulating among humans influenza subtypes A(h2N1) and A(h4N2). A(h2N1) is also denoted as A(h2N1)pdm09because he called pandemic of 2009 and subsequently replaced the seasonal influenza A(h2N1) virus that circulated until 2009 of the year. Only influenza A viruses are known to have caused pandemics. on the line. Type B influenza viruses currently circulating belong to the lines B/Yamagata and B/Victoria.
Influenza C virus is less common and usually results in mild infections. Therefore, it does not pose a problem for the public healthcare.
Group D viruses , mainly infect large cattle. According to available data, they do not infect people and do not cause them diseases.
Seasonal flu is characterized by sudden onset of high fever, cough (usually dry), headache, muscle and joint pain, severe malaise, sore throat and runny nose. The cough can be severe and last 2 weeks or more. In most people, the temperature returns to normal and symptoms resolve within a week without any medical attention. But influenza can lead to severe illness and death, especially in high-risk people (see below).
The disease can be mild or severe and even fatal. Hospitalizations and deaths occur mainly in high-risk groups. Annual influenza epidemics are estimated to result in 3-5 million cases of severe illness and 290,000 to 650,000 deaths from respiratory diseases.
In industrialized countries, the majority of influenza-related deaths occur among people aged 65 and older (1). Epidemics can lead to high levels of absenteeism from work/school and loss of productivity. During peak periods of illness, clinics and hospitals can be overcrowded.
Epidemics can lead to high levels of absenteeism from work/school and loss of productivity. During peak periods of illness, clinics and hospitals can be overcrowded.
The impact of seasonal influenza epidemics in developing countries is not well known, but studies show that 99% of influenza-associated lower respiratory tract infection deaths in children under 5 years of age occur in developing countries (2).
People get the flu at any age, but there are populations at increased risk .

Transmission of seasonal influenza occurs easily and quickly, especially in crowded places, including schools and boarding schools. When an infected person coughs or sneezes, small droplets containing the virus (infectious droplets) enter the air and can spread up to one meter and infect nearby people who inhale them. The infection can also be transmitted through hands contaminated with influenza viruses. Cover your mouth and nose with a tissue and wash your hands regularly to prevent transmission of infection when you cough.
In temperate areas seasonal epidemics occur mainly during the winter season, while in tropical areas influenza viruses circulate all year round, resulting in less regular epidemics. Seasonal epidemics and the burden of disease
The time period from infection to disease development, known as the incubation period , lasts about 2 days, but can vary from 1 to 4 days.
In most cases, human influenza is clinically diagnosed. However, during periods of low activity of influenza viruses and in the absence of epidemics, infection with other respiratory viruses such as rhinovirus, respiratory syncytial virus, parainfluenza virus, and adenovirus can also present as an influenza-like illness, making it difficult to clinically differentiate influenza from other pathogens.
Definitive diagnosis requires collection of appropriate respiratory specimens and a laboratory diagnostic test. The first critical step for laboratory detection of influenza virus infections is the proper collection, storage and transport of respiratory specimens. Typically, laboratory confirmation of influenza viruses in throat, nasal and nasopharyngeal secretions or aspirates or tracheal washes is by direct antigen detection, virus isolation, or detection of influenza-specific RNA by reverse transcriptase polymerase chain reaction (RT-PCR). There are a number of manuals on laboratory procedures published and updated by WHO (3).
Rapid diagnostic tests are used in clinics to detect influenza, but compared to RT-PCR methods, they have low sensitivity, and the reliability of their results depends largely on the conditions in which they are used.
Patients who are not at high risk should receive symptomatic treatment. If they have symptoms, they are advised to stay at home in order to minimize the risk of infecting others in the community. Treatment is aimed at alleviating flu symptoms, such as high fever. Patients should monitor their condition and seek medical attention if it worsens. If patients are known to be at high risk of developing severe illness or complications (see above), they should receive antivirals as soon as possible in addition to symptomatic treatment.
Patients with severe or progressive clinical disease associated with suspected or confirmed influenza virus infection (eg, clinical syndromes of pneumonia, sepsis, or exacerbation of comorbid chronic diseases) should receive antivirals as soon as possible.
WHO GISRS monitors antiviral drug resistance among circulating influenza viruses in order to provide timely guidance on the use of antivirals for clinical management and potential chemoprevention.
The most effective way to prevent the disease is vaccination . For more than 60 years, safe and effective vaccines have been available and used. Some time after vaccination, immunity weakens, so annual vaccination is recommended to protect against influenza. Injectable inactivated influenza vaccines are the most widely used in the world.
In healthy adults, influenza vaccine provides protection even if the circulating viruses do not exactly match the vaccine viruses. However, for older people, influenza vaccination may be less effective in preventing the disease, but it reduces the severity of the disease and reduces the likelihood of complications and death. Vaccination is especially important for people who are at high risk of developing complications and for people who live with or care for high-risk people.
WHO recommends annual vaccination for the following populations:

The effectiveness of an influenza vaccine depends on how well the circulating viruses match those contained in the vaccine. Due to the constantly changing nature of influenza viruses, the WHO Global Influenza Surveillance and Response System (GISRS), a system of national influenza centers and WHO collaborating centers around the world, continuously monitors influenza viruses circulating in humans and updates them twice a year. composition of influenza vaccines.
Over the years, WHO has been updating its recommendations for vaccine composition (trivalent) targeting the 3 most common circulating virus types (two influenza A subtypes and one influenza B subtype). Starting with the 2013-2014 influenza season in the northern hemisphere, a fourth component is recommended to facilitate the development of a quadrivalent vaccine. Quadrivalent vaccines include a second type B influenza virus in addition to the viruses in the trivalent vaccine and are expected to provide broader protection against influenza type B infections. Many inactivated and recombinant influenza vaccines are available in injectable form. A live attenuated influenza vaccine is available as a nasal spray.
Many inactivated and recombinant influenza vaccines are available in injectable form. A live attenuated influenza vaccine is available as a nasal spray.
Pre-exposure and post-exposure prophylaxis with antivirals is possible, but its effectiveness depends on a number of factors such as the individual, the type of exposure and the risk associated with the exposure.
In addition to vaccination and antiviral treatment, public health measures include personal protective measures such as:
WHO, through the WHO GISRS and in collaboration with other partners, monitors influenza activity globally, recommends bi-annual seasonal influenza vaccine formulations for northern and southern hemispheres, and assists countries with tropical and subtropical climates in the choice of vaccine preparations (for the northern and southern hemispheres) and decisions on the timing of vaccination campaigns, and provides support to Member States in the development of prevention and control strategies.