Thursday, May 18, 2017, 01:58 AM | Source: The Conversation
Kate Leslie, Megan Allen
Feeling tired or being unable to concentrate is common even days after surgery. But there are simple ways to help speed up your recovery. Jason Jones/Flickr, CC BYYou have a small operation under general anaesthesia and go home the same day. Two days later you’re back at work, but you can’t concentrate and have a desperate desire to take a nap. Why does this happen and how can you prevent it?
General anaesthesia is a reversible drug-induced coma, during which you are unconscious, don’t feel pain and don’t remember anything. This is precisely what you want when you’re having an invasive or painful procedure.
However, some people suffer lingering effects in the days after anaesthesia. These include drowsiness, slowed reaction times, and difficulty concentrating, remembering new information and finishing complex tasks.
Thankfully, these unwanted effects usually wear off by the next day, but sometimes they last for a few more days or even weeks. Then they can really disrupt your ability to work or get anything done at home.
The effects of general anaesthesia may appear to linger for days after surgery for many reasons. Tiredness after a procedure is commonly attributed to anaesthetics. But modern anaesthetics wear off completely in a couple of hours, so the real picture is usually more complicated.
The surgical condition for which you had the procedure may have stopped you leading a full and active life for some time, resulting in lack of fitness and less reserve for recovery.
The surgery itself causes tissue injury. After surgery, your body undergoes repair and recovery, which drives a higher baseline metabolic rate and draws on your nutrient stores. So it isn’t surprising such intense activity at a cellular level results in feeling tired after surgery.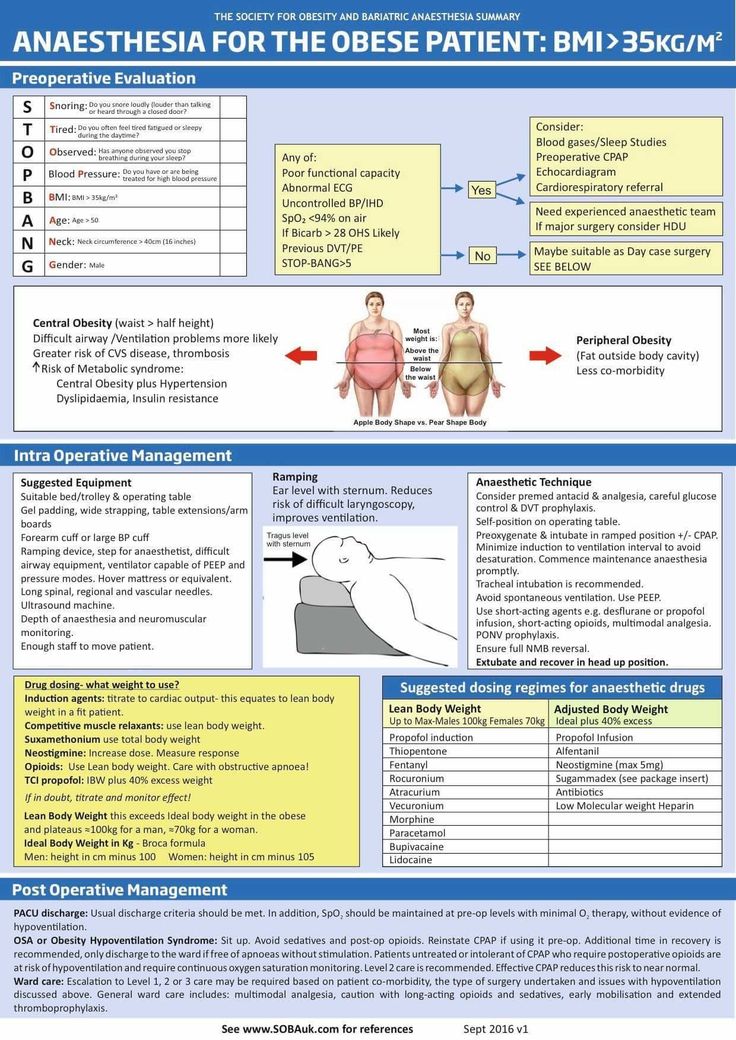
If you ignored your doctor’s advice to take it easy before or after surgery, that could also explain why you’re feeling tired.
Then there’s pain treatment before and after the procedure, which can also contribute to grogginess.
Strong painkillers you take before or after surgery, like oxycodone, can also make you feel drowsy. But side effects cease once you stop taking them. from www.shutterstock.comFor instance, opioids (such as oxycodone) and gabapentinoids (such as pregabalin) are strong pain medicines often prescribed after surgery. They are important in ensuring a comfortable recovery and rapid return to normal life, but may result in grogginess and confusion, especially in higher doses.
Opioids are usually needed for only a few days after surgery and these side effects stop when you stop taking them.
Finally, general anaesthetics interfere with your body clock. This could be because anaesthetics interfere with brain hormones, such as melatonin, and messenger chemicals called neurotransmitters.
While melatonin tablets can treat jet lag, which is also a disruption of the body clock, there is no good evidence to use melatonin for anaesthesia-induced body-clock disruption in humans.
An operation is a major life event. Make sure you get adequate rest and have enough support at work and home before your surgery.
A bit of anxiety is normal before surgery and can also be exhausting. You can reduce your anxiety by asking for clear explanations of what to expect, and by maintaining a warm, comfortable and calm waiting environment.
If you are very anxious, your anaesthetist can give you a sedative “pre-med” before you go to theatre. But the use of sedatives is a balancing act, as the calming effect before the procedure is desirable but not the “hangover” drowsiness afterwards, which may last for several hours.
Your anaesthetist is the medically trained specialist who can not only give you a “pre-med” but will look after you during your operation and plan your recovery.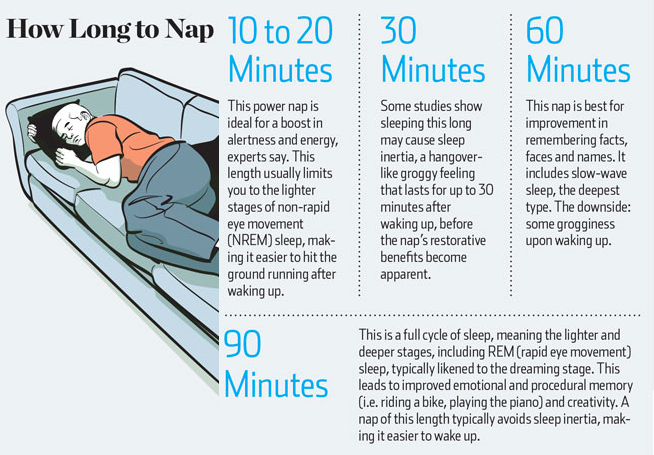 He or she will develop an individualised anaesthetic plan based on short-acting anaesthetics and a combination of pain-killings drugs.
He or she will develop an individualised anaesthetic plan based on short-acting anaesthetics and a combination of pain-killings drugs.
Your anaesthetist will also advise you how to best control your pain after surgery and when you return home. This will often involve using simple pain medicines, such as paracetamol and anti-inflammatory drugs, as well as opioids, which you will need to treat strong pain. Using simple pain medicines will help to reduce the doses of opioids that you need, and help you to avoid the nausea, constipation and grogginess that goes with them.
After a procedure, you can combat the disruption to your body clock by practising good “sleep hygiene”. This involves maximising cues to the body that it is time to sleep in the evening. These could include avoiding stimulants like caffeine and alcohol, going to bed at a similar time each night, being in a dimly lit room and engaging in calming or restful activities before sleep, like reading.
Making sure you are exposed to bright sunshine during the day and avoiding back-lit screens on technology devices in the evening can also help.
Lingering grogginess after general anaesthesia is hardly ever sinister. But if it is persistent, getting worse rather than better, or is associated with confusion, weakness or numbness, then you must see your doctor.
The authors do not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and have disclosed no relevant affiliations beyond their academic appointment.
Megan Allen Critical Care
Kate Leslie Critical Care
You have a small operation under general anaesthesia and go home the same day. Two days later you’re back at work, but you can’t concentrate and have a desperate desire to take a nap. Why does this happen and how can you prevent it?
Why does this happen and how can you prevent it?
General anaesthesia is a reversible drug-induced coma, during which you are unconscious, don’t feel pain and don’t remember anything. This is precisely what you want when you’re having an invasive or painful procedure.
However, some people suffer lingering effects in the days after anaesthesia. These include drowsiness, slowed reaction times, and difficulty concentrating, remembering new information and finishing complex tasks.
Thankfully, these unwanted effects usually wear off by the next day, but sometimes they last for a few more days or even weeks. Then they can really disrupt your ability to work or get anything done at home.
The effects of general anaesthesia may appear to linger for days after surgery for many reasons. Tiredness after a procedure is commonly attributed to anaesthetics. But modern anaesthetics wear off completely in a couple of hours, so the real picture is usually more complicated.
The surgical condition for which you had the procedure may have stopped you leading a full and active life for some time, resulting in lack of fitness and less reserve for recovery.
The surgery itself causes tissue injury. After surgery, your body undergoes repair and recovery, which drives a higher baseline metabolic rate and draws on your nutrient stores. So it isn’t surprising such intense activity at a cellular level results in feeling tired after surgery.
If you ignored your doctor’s advice to take it easy before or after surgery, that could also explain why you’re feeling tired.
Then there’s pain treatment before and after the procedure, which can also contribute to grogginess.
Strong painkillers you take before or after surgery, like oxycodone, can also make you feel drowsy. But side effects cease once you stop taking them. from www.shutterstock.comFor instance, opioids (such as oxycodone) and gabapentinoids (such as pregabalin) are strong pain medicines often prescribed after surgery. They are important in ensuring a comfortable recovery and rapid return to normal life, but may result in grogginess and confusion, especially in higher doses.
They are important in ensuring a comfortable recovery and rapid return to normal life, but may result in grogginess and confusion, especially in higher doses.
Opioids are usually needed for only a few days after surgery and these side effects stop when you stop taking them.
Finally, general anaesthetics interfere with your body clock. This could be because anaesthetics interfere with brain hormones, such as melatonin, and messenger chemicals called neurotransmitters.
While melatonin tablets can treat jet lag, which is also a disruption of the body clock, there is no good evidence to use melatonin for anaesthesia-induced body-clock disruption in humans.
An operation is a major life event. Make sure you get adequate rest and have enough support at work and home before your surgery.
A bit of anxiety is normal before surgery and can also be exhausting. You can reduce your anxiety by asking for clear explanations of what to expect, and by maintaining a warm, comfortable and calm waiting environment.
If you are very anxious, your anaesthetist can give you a sedative “pre-med” before you go to theatre. But the use of sedatives is a balancing act, as the calming effect before the procedure is desirable but not the “hangover” drowsiness afterwards, which may last for several hours.
Your anaesthetist is the medically trained specialist who can not only give you a “pre-med” but will look after you during your operation and plan your recovery. He or she will develop an individualised anaesthetic plan based on short-acting anaesthetics and a combination of pain-killings drugs.
Your anaesthetist will also advise you how to best control your pain after surgery and when you return home. This will often involve using simple pain medicines, such as paracetamol and anti-inflammatory drugs, as well as opioids, which you will need to treat strong pain. Using simple pain medicines will help to reduce the doses of opioids that you need, and help you to avoid the nausea, constipation and grogginess that goes with them.
After a procedure, you can combat the disruption to your body clock by practising good “sleep hygiene”. This involves maximising cues to the body that it is time to sleep in the evening. These could include avoiding stimulants like caffeine and alcohol, going to bed at a similar time each night, being in a dimly lit room and engaging in calming or restful activities before sleep, like reading.
Making sure you are exposed to bright sunshine during the day and avoiding back-lit screens on technology devices in the evening can also help.
Lingering grogginess after general anaesthesia is hardly ever sinister. But if it is persistent, getting worse rather than better, or is associated with confusion, weakness or numbness, then you must see your doctor.
Apparatus with everything necessary for anesthesia in children.
There is such a wonderful phobia among people who encountered Soviet punitive dentistry in childhood - stomatophobia. Then it was believed that local anesthesia was invented for the weak in spirit, and it was normal to endure the smell of burnt dentin and terrible pain for an hour. Despite the fact that no sane dentist would now treat without anesthesia, sad sad people still walk among us, traumatized by these memories. Sometimes such patients overpower themselves and come to the appointment with a panoramic picture of the teeth. More precisely, with a dozen dilapidated roots and many infected purulent foci in the bone structure of the jaw.
Then it was believed that local anesthesia was invented for the weak in spirit, and it was normal to endure the smell of burnt dentin and terrible pain for an hour. Despite the fact that no sane dentist would now treat without anesthesia, sad sad people still walk among us, traumatized by these memories. Sometimes such patients overpower themselves and come to the appointment with a panoramic picture of the teeth. More precisely, with a dozen dilapidated roots and many infected purulent foci in the bone structure of the jaw.
If people have gotten used to the idea that children must be treated under local anesthesia, then general anesthesia is still scary. Many still remember the difficult exit from anesthesia with nausea and “helicopters” during the use of heavy old drugs. And until now, people have a feeling that any general anesthesia is something extremely dangerous and even more unacceptable for use in children, except for emergency indications. In fact, things have changed a lot.
In short, let's talk about anesthesia in children. And also about modern options with nitrous oxide, propofol and sevoflurane. They are very good, but remember that independent experiments with them may end up meeting Kurt Cobain.
Let's take a look at what anesthesia is. Our brain is a complex set of neurons that are constantly exchanging impulses with each other. Some substances can inhibit synaptic transmission between individual groups of neurons. Moreover, different substances have different mechanisms of action and their own characteristics. In fact, anesthesia is also one of the varieties of anesthesia. Only in contrast to the local shutdown of local pain neurons with local anesthesia, we partially “turn off the brain”.
As a result, general anesthesia is not like a complete "turn off" of the brain. It is rather a kind of very deep sleep, from which you can wake up only when the anesthesiologist allows it. What is suppressed first? For starters, it's consciousness. The main purpose of general anesthesia is to reduce the patient's stress level. We want to make sure that the whole treatment goes unnoticed for him and does not leave any unpleasant memories. In addition, pain sensitivity is suppressed and motor activity is inhibited. That is, with proper anesthesia, the patient does not hurt, and he does not try to get up and leave, portraying a sleepwalker.
What is suppressed first? For starters, it's consciousness. The main purpose of general anesthesia is to reduce the patient's stress level. We want to make sure that the whole treatment goes unnoticed for him and does not leave any unpleasant memories. In addition, pain sensitivity is suppressed and motor activity is inhibited. That is, with proper anesthesia, the patient does not hurt, and he does not try to get up and leave, portraying a sleepwalker.
Of course, the suppression of the CNS functions should turn off only consciousness and pain, without affecting the important autonomous centers for the regulation of heartbeat, respiration, and vascular tone. Correctly all this can be provided only by experienced doctors. Usually there are four degrees of anesthesia depth:
If necessary, the anesthesiologist can vary the degree of CNS depression, for example, to ask the patient to move the jaw correctly. This can be done when using propofol, for example. Or, conversely, increase the depth if the patient began to worry.
This can be done when using propofol, for example. Or, conversely, increase the depth if the patient began to worry.
Why are such methods needed at all, if there is a conditional local articaine, which most often can be dispensed with? The problem in the first place is panic fear and stomatophobia. A good patient is a calm patient, not one who tries to run away in horror and flinches at every movement of the doctor. This will not benefit the patient himself and will not help the doctor to cure him qualitatively. Additional arguments in favor of anesthesia will be a very pronounced gag reflex and a large amount of intervention. We can't just anesthetic a patient, especially a small one. A local anesthetic also has dosage limits for simultaneous administration, and, for example, bilateral conduction anesthesia in the lower jaw can cause breathing difficulties due to the complete loss of tongue sensitivity. Well, and most importantly, even the most sensitive doctor will never agree with a child on the treatment of 15-20 teeth at the same time.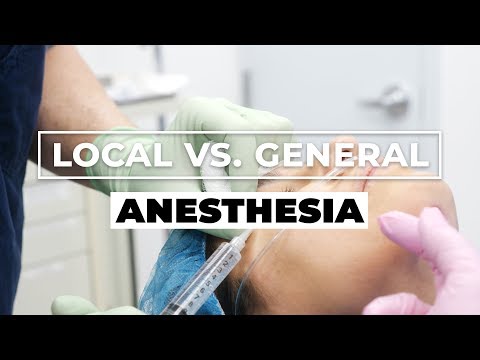 Yes, it also happens when children do not brush their teeth normally, eat buns and do not go to the dentist.
Yes, it also happens when children do not brush their teeth normally, eat buns and do not go to the dentist.
Therefore, oddly enough, it is general anesthesia that can often be an easier and more comfortable choice for a small patient and the attending physician.
Before we go into detail about how we use general anesthesia in children, let's go over a few key drugs. These are nitrous oxide, propofol, and sevoflurane (better known by the commercial name "Sevoran"). Without them, it is difficult to imagine modern safe general anesthesia with easy and quick awakening.
The correct use of modern methods is very important for the child to easily endure anesthesia.
Nitrous oxide has long been known solely as "laughing gas".
The history of the medical use of nitrous oxide began in 1799, when sophomore Humphry Davy, who became an eminent scientist, drew attention to the fact that inhalation of this gas causes euphoria and intoxication. In the process of experiments, he accidentally drew attention to the fact that under the influence of gas, toothache disappears. Don't ask me what those experiments were. In 1844, Horace Wells performed the first dental operations under nitrous oxide anesthesia. Now it is one of the most common gases used to relieve pain sensitivity during small manipulations.
In the process of experiments, he accidentally drew attention to the fact that under the influence of gas, toothache disappears. Don't ask me what those experiments were. In 1844, Horace Wells performed the first dental operations under nitrous oxide anesthesia. Now it is one of the most common gases used to relieve pain sensitivity during small manipulations.
Nitrous oxide has virtually no toxic effects when used correctly. It is metabolized: 99.996% of the gas is excreted during exhalation unchanged. Because of this, its effects are very short-lived and most often wear off within a minute of stopping the supply. Its safety profile is so good that it is used for pain relief in children and pregnant women during childbirth. In the second case, it is used in the so-called "anesthesia on demand" mode, when a woman in labor, before the onset of a contraction, takes several breaths of a mixture of nitrous oxide and oxygen from a mask of a special apparatus. In this case, the fight is almost painless. Not as effective as epidural anesthesia, but much faster.
Not as effective as epidural anesthesia, but much faster.
The main effects are achieved due to the antagonistic action on NMDA receptors. Many synthetic opiates, such as tramadol, work in a similar way. But unlike opiates, nitrous oxide is not addictive and does not suppress the respiratory center, which contributes to its high safety profile. Also, through a mechanism that is not entirely clear, endorphins are released, which triggers our internal mechanism for limiting pain sensations - the antinociceptive system. At the same time, the analgesic effect is quite strong and is approximately equivalent in strength to 15 mg of morphine. But nitrous alone is not enough to do anything with the teeth, so it is used in combination with local anesthesia.
Mild euphoria and increased mood are achieved by stimulating the release of dopamine, according to rat experiments.
It also has an anxiolytic effect: it suppresses anxiety. In small doses, nitrous oxide increases the sensitivity of GABAA receptors. Anti-anxiety drugs from the benzodiazepine group work in much the same way. As a result, the patient's anxiety decreases, he relaxes and shows slight drowsiness. There is also a slight anticonvulsant effect.
Anti-anxiety drugs from the benzodiazepine group work in much the same way. As a result, the patient's anxiety decreases, he relaxes and shows slight drowsiness. There is also a slight anticonvulsant effect.
An overdose as such is also almost impossible. The main key point that needs to be monitored is the saturation of the patient in order to exclude oxygen starvation. Well, if there is no anesthesiologist nearby and the action takes place in a nightclub - so that the patient does not have time to play tricks and hit during his attack of Viking madness on protruding objects and guards.
Quick summary: Treating teeth with nitrous oxide is fun and safe, as long as it doesn't involve very deep interventions. Then the pain still breaks through.
Ampoule with propofol emulsion.
Propofol is another significant drug in the practice of an anesthesiologist. The drug has a milky white color due to the fact that it is not a solution, but an emulsion. The active substance itself is insoluble in normal saline, therefore it is administered as a stabilized emulsion with a phospholipid base.
The active substance itself is insoluble in normal saline, therefore it is administered as a stabilized emulsion with a phospholipid base.
The drug works interestingly. Surely you have seen how in films the patient is injected with something, and he instantly turns off. Propofol has exactly the same effect. Our brain is largely composed of fats, in which propofol is highly soluble. Therefore, the time from its introduction to loss of consciousness is only a few seconds. It takes just a few heartbeats to deliver the right dose of the drug to the central nervous system.
Interestingly, propofol has only a sedative effect, inhibiting CNS activity. At the same time, it does not suppress pain and tactile sensitivity. Therefore, it must be combined with local anesthetics. And he also has a very funny feature: he causes retrograde amnesia, that is, the last thing the patient remembers after waking up is the events shortly before the injection of the drug. Moreover, similarly to sodium thiopental, propofol allows you to control patients to perform the simplest commands: stick out your tongue, close your mouth, open your mouth. That is, some contact is maintained, which is a big plus in some situations. Actually, it was precisely for this combination of amnesia and controllability that the same sodium thiopental was described in all spy novels as “truth serum”. In fact, a real interrogation would be difficult to conduct, since the patient would most likely just mumble something incoherent.
That is, some contact is maintained, which is a big plus in some situations. Actually, it was precisely for this combination of amnesia and controllability that the same sodium thiopental was described in all spy novels as “truth serum”. In fact, a real interrogation would be difficult to conduct, since the patient would most likely just mumble something incoherent.
Just propofol - you feel everything, it hurts, you follow simple commands and you can even mumble incoherently: "Fuck off, I'm married," but then you forget everything. Propofol + topical removes the pain from this situation, but you twitch and interfere with the doctor, your pulse can dangerously accelerate when you make an incision. Propofol + the same sevoran remove the pain and allow you to control the situation completely, but even turn off the level of consciousness that allowed you to mumble.
Pleasantly sweet-smelling gas with a common commercial name "Sevoran" is one of the most convenient and safe options for inhalation anesthesia, replacing halothane and isoflurane in modern anesthesiology. It has become widespread due to its excellent safety profile and easy induction and recovery from anesthesia. With its advent, the typical "helicopters" with vomiting long hours after the operation, characteristic of past generations of drugs, are a thing of the past.
It has become widespread due to its excellent safety profile and easy induction and recovery from anesthesia. With its advent, the typical "helicopters" with vomiting long hours after the operation, characteristic of past generations of drugs, are a thing of the past.
Due to moderate relaxation of the respiratory muscles and general sedation, it suppresses the trigger zones of the cough and gag reflexes. This means that the doctor can work calmly without fear that the patient suddenly starts to feel sick or coughs during subtle manipulations (for which he is especially loved by gastroenterologists with EGD). In this case, the anesthesiologist continuously monitors the pressure and blood saturation of the patient. This is important to avoid even the slightest lack of oxygen supply even in the smallest of patients.
The laryngeal mask is inserted like this.
It is most often used in combination with nitrous oxide and oxygen for anesthesia. When the patient falls asleep, the face mask is changed to a laryngeal one. Further, the patient's breathing is controlled by the ventilator. At the same time, the introduction of a laryngeal mask for inhalation anesthesia in children differs from that in adults. Children have a different structure of the larynx and other angles of introduction. For example, we always take into account the characteristics of children with a relatively short neck or malocclusion. A good doctor working with children will do this as gently as possible - so that the child will not have any discomfort in the larynx after waking up.
When the patient falls asleep, the face mask is changed to a laryngeal one. Further, the patient's breathing is controlled by the ventilator. At the same time, the introduction of a laryngeal mask for inhalation anesthesia in children differs from that in adults. Children have a different structure of the larynx and other angles of introduction. For example, we always take into account the characteristics of children with a relatively short neck or malocclusion. A good doctor working with children will do this as gently as possible - so that the child will not have any discomfort in the larynx after waking up.
So, we went over the main properties of drugs for general anesthesia. Now let's look at which options are better in each case. No children are the same, they are all different. Some child will calmly react to the placement of a catheter at a very young age, and some will refuse a painless mask at the age of eight or nine. Therefore, we always carefully communicate with both the baby and his parents. This is necessary to establish a trusting contact between the doctor and the little patient. Without this, it simply won't work properly. In parallel, the most detailed information is collected on the characteristics of the child's health, so that the anesthesiologist can choose the most comfortable and safe option for him in general anesthesia.
Therefore, we always carefully communicate with both the baby and his parents. This is necessary to establish a trusting contact between the doctor and the little patient. Without this, it simply won't work properly. In parallel, the most detailed information is collected on the characteristics of the child's health, so that the anesthesiologist can choose the most comfortable and safe option for him in general anesthesia.
Interestingly, children very quickly begin to trust doctors if they see that everything went painlessly, and the tooth no longer bothers them. As a rule, further treatment is much easier. We had a case when a girl fell off a swing in a kindergarten, hit herself and lost an artificial crown, which she had to put almost three of us. As a result, she herself returned to the clinic with her parents, brought the crown in her palm and asked to return it to its place.
Best for : Brave kids of all ages who trust a doctor.
This option is a bit off topic of our post, but I also want to mention it. If the child initially comes with a bunch of affected teeth, and even for some reason intimidated by relatives, then such a scenario may not be possible. And you need to treat. This is where the whole arsenal of general anesthesia tools will help us.
The child should be able to breathe freely through the nose. Nitrous oxide has a bunch of effects that we need. It relaxes, eliminates anxiety, slightly cheers up. During treatment, the patient will be conscious. At the same time, it will not work in its pure form to anesthetize, it will still be painful to dissect teeth. Therefore, we usually let the child breathe through a special mask that covers only the nose. A lot of people really like it, plus we often tell stories about test pilots who also have special masks with a breathing mixture.
When the child is relaxed, it is possible to apply anesthesia with gel and then inject the main anesthetic. Unfortunately, under nitrous oxide it will not be possible to do a large amount of intervention at once. Children get tired of lying with their mouths open, the mask becomes annoying. Therefore, this method is better suited for small simultaneous interventions - one or two teeth. At the same time, we cannot increase the concentration above 50% for a child; we need to look for other, stronger, but safe drugs.
Unfortunately, under nitrous oxide it will not be possible to do a large amount of intervention at once. Children get tired of lying with their mouths open, the mask becomes annoying. Therefore, this method is better suited for small simultaneous interventions - one or two teeth. At the same time, we cannot increase the concentration above 50% for a child; we need to look for other, stronger, but safe drugs.
Sevoflurane can be given to school-age children without any problems, but there are several nuances. With older children, it is easier to arrange for local anesthesia in the mind or for the use of propofol with intravenous administration. There are several advantages to completely turning off consciousness, which does not happen with the same nitrous oxide.
Firstly, the child does not experience wild stress and does not earn dental phobia for the rest of his life. There is nothing worse than a stern nurse who kneels on you and holds a mouthpiece while the doctor frantically tries to do at least something in the oral cavity.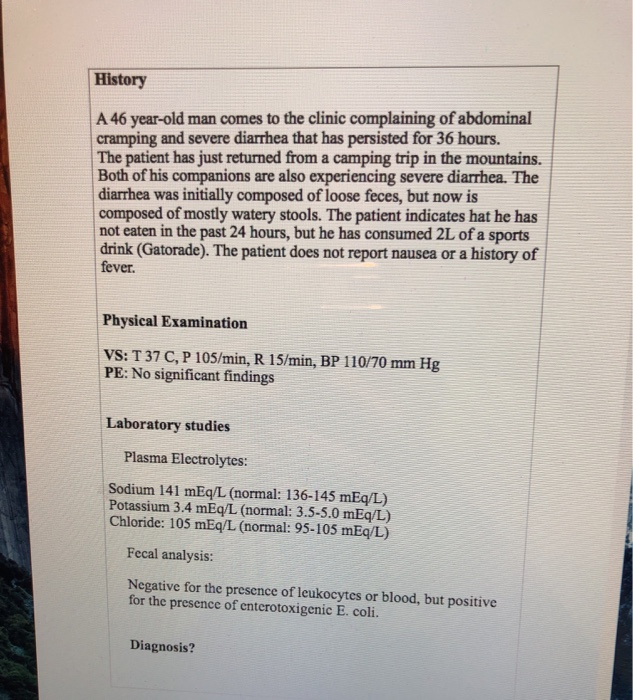
Secondly, it allows for high-quality treatment, when the doctor is sure that the patient will not twitch, will not start waving his tongue, will not try to run away in the middle of an important stage.
The anesthesiologist can vary the depth of anesthesia by changing the composition of the gas mixture. This makes it possible to accurately monitor the patient's vital signs and provide the desired level of relaxation and stillness. If you need to treat caries, then there is no point in injecting an additional anesthetic. The degree of CNS suppression is enough to make the patient comfortable. If it is planned to treat pulpitis or periodontitis, remove teeth, then we additionally introduce a local anesthetic. Otherwise, pain impulses will still reach the “sleeping” brain and cause an adrenaline rush and involuntary movements. With a complete shutdown of consciousness, we can carry out any amount of intervention. And we are talking not only about some painful things like treating six carious teeth in one go, but also, for example, about taking accurate impressions for the subsequent manufacture of orthopedic and orthodontic structures. Try convincing a sobbing four-year-old that he needs to sit still while the silicone in the impression tray hardens in his mouth.
Try convincing a sobbing four-year-old that he needs to sit still while the silicone in the impression tray hardens in his mouth.
A child under three years of age is not allowed to use it. We have already analyzed the features of propofol above. It does not have an analgesic effect, but only suppresses consciousness. That is why it must be supplemented with local anesthesia, as if the patient were awake. But its main advantage when working with the same teenagers is that they can follow simple commands. This makes the doctor's job easier. You can reduce the depth of anesthesia and ask to bite the template, model the bite design, or something similar. For a dentist, it is important not only to depict fillings in place of carious defects, but to carefully model the occlusal ratios of the jaws so that the chewing biomechanics is ideal after treatment.
No. And parents should not just tell the child about this, but make sure that he does not eat cookies from his secret reserves. The child is hungry, he will try to eat at least something. Anesthesia on a full stomach threatens to vomit during treatment or upon awakening. If it is "in the process of treatment", then the substance can block the airways, which no one needs.
And parents should not just tell the child about this, but make sure that he does not eat cookies from his secret reserves. The child is hungry, he will try to eat at least something. Anesthesia on a full stomach threatens to vomit during treatment or upon awakening. If it is "in the process of treatment", then the substance can block the airways, which no one needs.
If all the protocols are followed, the process is monitored by an experienced anesthesiologist, then everything goes without problems and any special side effects. To do this, we comply with all protocols and everything that is necessary for complete safety. For example, here is a study that suggests that with proper anesthesia with propofol and isoflurane, all side effects after waking up last less than a day.
But sometimes our hair just stands on end when a mother comes to our clinic after not having the right anesthesia in another place.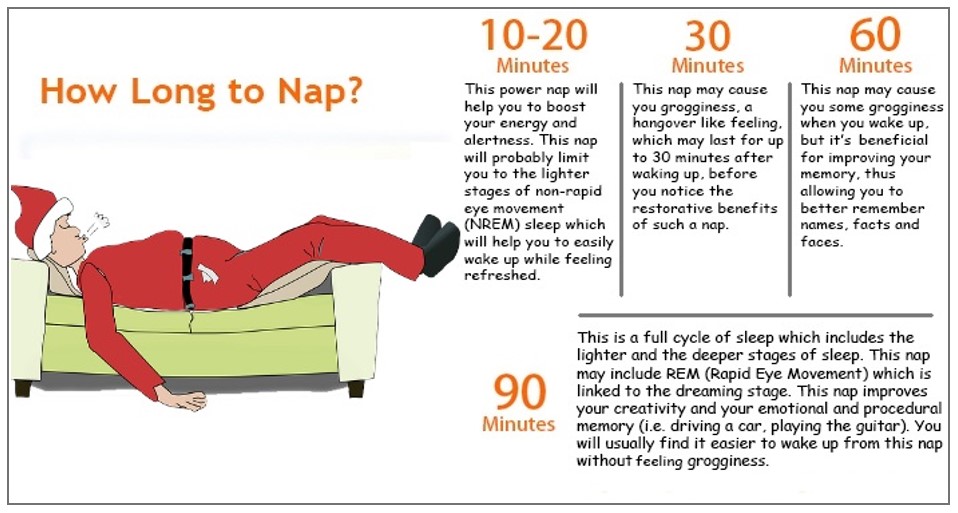 We usually catch these parents with a load of food for a week and the moral expectation of three days of continuous vomiting and dizziness after waking up. Here you immediately understand that in another place the general anesthesia was not entirely correct.
We usually catch these parents with a load of food for a week and the moral expectation of three days of continuous vomiting and dizziness after waking up. Here you immediately understand that in another place the general anesthesia was not entirely correct.
Yes. It's not a matter of probability, it's a matter of protocol. You need to check the equipment, have a doctor with the necessary qualifications, understand the characteristics of a particular patient. Then there will be no surprises. The process is closely monitored by an anesthesiologist-resuscitator, who is ready to intervene at any time and adjust the parameters of anesthesia. He knows how to smoothly introduce and withdraw from anesthesia, he knows all the nuances of resuscitation in children.
Yes, it happens. But I think that they are not quite right and they simply do not have a good anesthesiologist. The safety of general anesthesia for the health and mental abilities of the baby is confirmed by numerous studies. For example, they took 19,296 children and studied their development after many anesthesias, up to the age of 20. The results prove that everything is fine, and the children are no different from their peers. At the same time, many sources still come to the conclusion that repeated anesthesia under the age of two years is undesirable.
In general, sometimes misunderstanding and fear of general anesthesia take strange forms in some doctors. In my memory, there was one wild case when a doctor tried to save children from terrible anesthesia, replacing it with temporary suffocation with a towel. Binds, holds and heals half strangled. Such a good doctor. Moreover, in fact, she uses the variant of round anesthesia. But it was relevant several hundred years ago, when even ether anesthesia was not invented, and the only option for conditional amputation was a precisely calculated blow with a wooden mallet on the crown. But it was difficult to control the “depth” of such anesthesia and guarantee a successful awakening.
But it was difficult to control the “depth” of such anesthesia and guarantee a successful awakening.
The eyes dry only with deep anesthesia, in our case they are sufficiently moistened with a tear. The patient's eyelids are fixed with a special plaster. So the eyes remain closed, and the mucous membrane does not dry out. Well, there is no risk that something could get into them.
I know it sounds weird, but that's what parents ask. Here's the thing: if you lose a lot of blood during surgery, then hair loss can be a side effect. But when a mistake is made in surgery, it is most often attributed to uncontrollable factors in the spirit of: “This is such a drug for anesthesia,” and not to the fact that someone could not perform the manipulation on time or did not make the right decision. And the anesthesiologist has nothing to do with it.
It won't make a difference, either good or bad. The anesthesiologist carefully monitors the saturation level to ensure that the young brain receives enough oxygen. The device does not supply pure gas, but mixed with oxygen. All sensors are built into the ventilator. If necessary, the doctor can, for example, adjust the composition of the gas mixture. All drugs have an excellent safety profile and a bunch of studies confirming their safety when used in pediatric patients. And we can work quickly. If we used to work on very voluminous interventions for six hours, then up to four, up to three, now the average duration is no more than 2.5 hours: this, in particular, is why we need technology and a professional team.
Will not. The child will not remember the process of anesthesia itself and, most likely, some short period before it. Just try not to scare him once again: children are very impressionable. Then we will try to make everything as comfortable as possible for him: fell asleep, woke up, and then we also played.
Just try not to scare him once again: children are very impressionable. Then we will try to make everything as comfortable as possible for him: fell asleep, woke up, and then we also played.
The most difficult thing in dentistry is not to scare the child. Unfortunately, some strange grandparents often do this for us, who scare the child with doctors. Please don't ever tell your kids things like, “If you eat candy, you'll ruin your teeth. And then the doctor will drill your teeth with a terrible drill. Sooner or later, a small patient will have to face the dentist. And we would like him to trust us, and not run away screaming at the sight of a white coat. Otherwise, everything can end with persistent stomatophobia, a full mouth of prostheses and a bunch of problems for life.
In previous posts about palatal retractors and the scientific approach to dentistry, you asked about the clinic. If you want to treat your teeth with us, then say “I'm from Habr”, there will be a small 5% discount.
If you want to treat your teeth with us, then say “I'm from Habr”, there will be a small 5% discount.
So, you almost decided to do laser vision correction. But questions are still tormenting: what will the new vision be like? How quickly will it return to normal and what are the "pitfalls" during the rehabilitation period?
Let's talk!
You will feel the change in vision immediately after the operation is completed. Get up from the couch and suddenly, for example, make out the clock face in the operating room or the numbers on the wall calendar. But this may not impress you, because emotionally you are still there, under the guns of surgical instruments.
After a short rest, the doctor will examine your eyes again, measure your visual acuity, drip drops and let you go home. The doctor will also tell you about the rules in the rehabilitation period, write out a prescription and tell you what and how to drip correctly.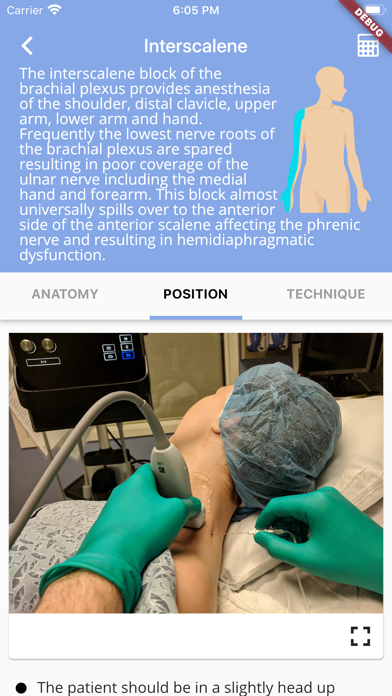 But often patients do not remember this well, so they are given a memo with them.
But often patients do not remember this well, so they are given a memo with them.
Take an escort with you! Let him remember everything. It will be difficult for you to read the memo on the first day after the operation.
The recovery phase after laser vision correction begins.
And immediately the first "pitfall": anesthesia has ceased to act and the eyes begin to react to the intervention. The laser vaporizes a negligible portion of the cornea, but it is still a burn. Soreness, itching, sensitivity to light may appear. Especially often such sensations appear after photorefractive keratectomy. The body tries to protect the wound surface, so tears flow so that the eye cannot be opened.
At first, after the correction, the eyes are very watery. This is how the protective function of the body manifests itself
Here again the escort will help out. And dark glasses! They will not only help from blinding light, but will create a barrier from wind and dust on the street. Be sure to take them with you.
Be sure to take them with you.
If there is no one to take you home, call a taxi.
We strongly advise against driving after the operation. This is dangerous.
Lights at home should be dimmed if possible. The first few hours the darkness is more comfortable for the eyes. Stars and glare may be observed. This is fine. They will soon go away on their own. If the pain persists and cannot be tolerated, take a pill of any pain reliever.
Most importantly, never touch or rub your eyes. Even through a closed eyelid. You also don't need to squint too hard. Gently pat your tears under your eyes with a tissue.
The first day after the operation, it is very important to exclude mechanical effects on the eye. The corneal flap, which was created during laser vision correction, may develop folds or may become displaced. This will adversely affect the quality of vision. I'll have to go back to the clinic and reposition the flap.
For the same reason, it is recommended to sleep on your back the first night.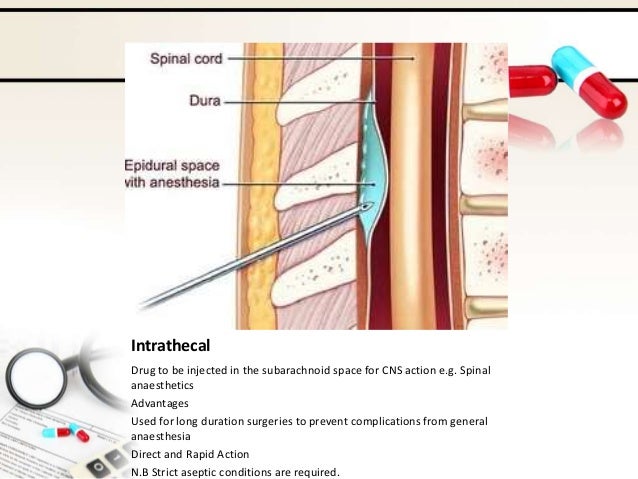 It is better to wear glasses so that you do not accidentally touch your eyes in a dream.
It is better to wear glasses so that you do not accidentally touch your eyes in a dream.
Blurred vision
In the morning, vision is likely to be blurry. Don't panic. Everything will be fine in an hour. The brain needs time to get used to the information that the eyes are now transmitting. From the intense work of the brain, a headache can appear.
Dry eye syndrome
Your eyes will dry out the next day. This is a natural reaction of the body to too much lacrimation the day before. Temporary dry eye syndrome develops in the vast majority of patients. It is accompanied by itching and a feeling of sand in the eyes. You still can't touch your eyes! Therefore, we do not wash. And we don't use makeup.
Ease the condition of the drugs that the doctor prescribed for you. Among them will be anti-inflammatory drops, tear substitutes, as well as vitamin complexes that improve tissue regeneration.
Dry eye syndrome is different for everyone. Someone for a week, someone else for six months continues to use drops. These are all variants of the norm. Much depends on the individual characteristics of the organism and on how much you will load your eyes.
Someone for a week, someone else for six months continues to use drops. These are all variants of the norm. Much depends on the individual characteristics of the organism and on how much you will load your eyes.
Help your eyes recover faster! The eyes need rest.
Take sick leave if the work is associated with factors unfavorable to the eyes. Put aside knitting, reading and watching TV for a while. Even from 5 minutes of surfing on the phone, dry eyes will noticeably increase.
Boring? Download audiobooks in advance, listen to music. Take a walk, but be sure to wear dark glasses.
Inflammation
Some patients report slight redness of the eyes the day after surgery. No need to be afraid. This is not inflammation, but microruptures of the capillaries of the eye in response to mechanical stress during laser correction. They will pass within a couple of days.
To prevent inflammation, the doctor will definitely prescribe antibiotics.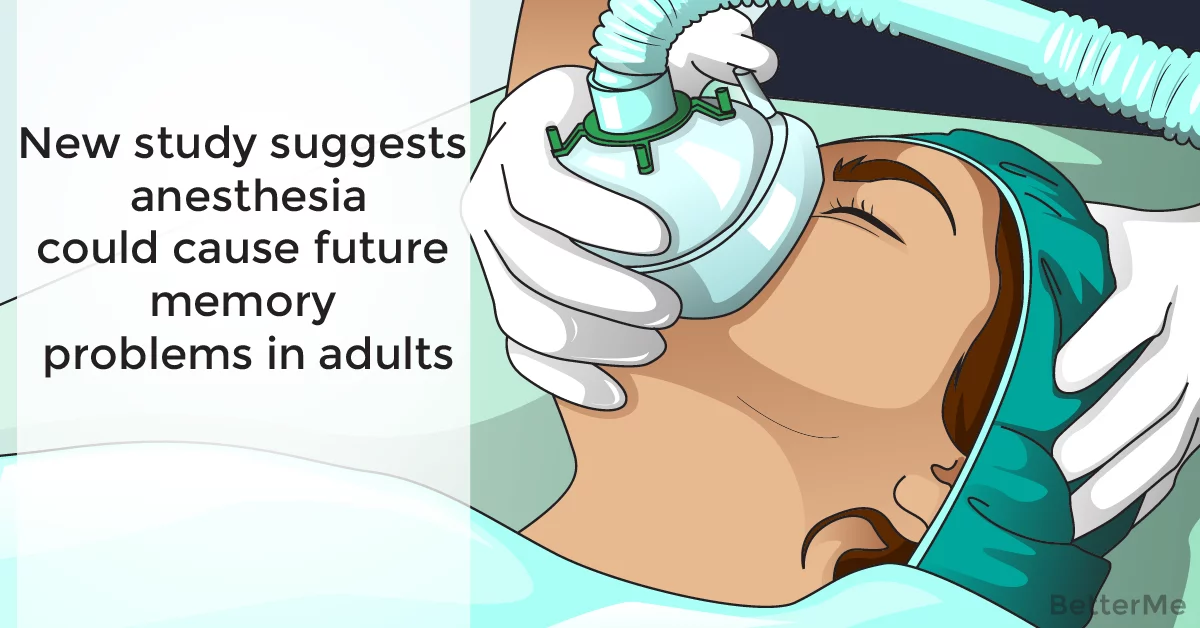 You need to drip them strictly according to the scheme, in the indicated dosage. The wound on the cornea has not yet healed and is very vulnerable to infections.
You need to drip them strictly according to the scheme, in the indicated dosage. The wound on the cornea has not yet healed and is very vulnerable to infections.
Your new vision is starting to please you! The whole world, familiar things, relatives now look different, brighter, clearer. How many details now you can see! Starting from the grains on the pavement, and to the pattern on the curtains in the windows of a neighboring house.
It will seem that your vision is even more than unity. But it's hard to focus up close. Be patient. These are the stages of vision stabilization. The left and right eyes may see differently. Everything will be back to normal soon.
While vision stabilizes, the right and left eyes can see differently. This is fine.
Do not try to evaluate the results of laser vision correction by the first sensations!
Vision will be unstable for about a month. But every day the positive dynamics will be more and more.
A week later, rehabilitation after laser vision correction is in full swing. In the morning, the eyes “turn on to work” faster and see better and better, you can spend an hour or even two at the computer, with breaks even longer. Drops have to drip less often. The new vision becomes habitual. Life is getting back to normal.
However, full recovery of the eyes after laser vision correction has not yet occurred. It is important not to weaken discipline and continue to responsibly observe the necessary rules:
Physical activity and high temperatures, albeit temporarily, overload the body, and this will immediately affect the quality of vision. If your job involves lifting weights, it's best to take a vacation.
But the eyes now need more than just rest. Simple exercises after vision correction will help them quickly adapt to new optical characteristics.
Simple exercises after vision correction will help them quickly adapt to new optical characteristics.
Payload on the eyes
Starting from the second week after surgery, you can perform simple but effective exercises to train the eye muscles responsible for near and far vision.
To do this, you need to alternately focus your eyes on objects located at different distances. Several times for 3-4 sets with breaks. Nothing complicated - a minute or two of your time, but it is advisable to do them periodically during the day.
At the computer, get distracted more often and look out the window.
If you feel tension in your eyes, do palming. Cover your eyes with cupped palms and sit like that for a while. The warmth of the hands and the darkness will relieve fatigue and improve color perception.
Some special gymnastics for recovery after laser vision correction in most cases is not required. Vision gradually normalizes itself.
If it becomes necessary to maintain or maintain the quality of vision with the help of special exercises, the doctor will prescribe them after the final completion of the rehabilitation course. Not earlier than one month after the operation.
Not earlier than one month after the operation.
Therefore, do not neglect follow-up visits to the ophthalmologist after the operation.
On average, one month after laser vision correction, the main stage of recovery is completed. You can evaluate the results.
Evening and night vision may still not be ideal, as it takes longer to recover - from 3 months to six months. But if you do not get involved in night driving, then this will not cause much discomfort.
Most patients return to their usual way of life and use their new vision with pleasure. They remember the trials they experienced easily and do not regret that they decided to have an operation.
If after a month your vision begins to deteriorate, be sure to consult a doctor. Perhaps the problem is not related to the correction of refraction, but to other diseases that were not clearly expressed at the stage of preparation for the operation.