• 21
By GRACE CORDOVANO, DEVEN McGRAW, and AARON MIRI
The HIPAA Privacy Rule gives patients the right to copies of their medical records, with rare exceptions. When patients need a copy of their medical records, most start the process by calling their doctor’s office and asking for how to get access. The receptionist or office staff point them in the right direction, whether it’s instructing them to write down their request and sending it to the office, pointing them to contact the medical records or radiology department (if the practice is large enough), or assisting them in setting up their patient portal, if the practice is using an electronic health record (EHR). Being able to connect with a person inside the four walls of medicine is often crucial for many patients and their carepartners who may be unsure of exactly how to request their records.
But what happens to those records when a doctor closes or leaves the practice?
Independent practices close for a variety of reasons. Physicians may merge with a large practice or health system, retire, they may sell or close their practice for personal reasons, they may file for bankruptcy, or they may get sick and die. The COVID19 pandemic has had devastating financial consequences on many small, independent, and rural practices, leading to their consequent closure, acquisition, or merger.
What should patients do when their doctor’s office closes, and they need a copy of their medical records? This is especially challenging when a doctor may not have had an EHR, as is the case with many independent practices as well as more rural settings. On September 26, 2020, a tweet from Cait DesRoches, Executive Director of OpenNotes, inquired about how a family member may get access to medical records from her physican’s practice that closed, triggering a robust conversation that led to the realization that patients and families are not well informed in these circumstances.
Prevention is Worth a Pound of Cure
It can be much more difficult to get copies of records after a practice has closed. Patients should get copies of their medical records as they are generated instead of waiting until they’re needed. HIPAA Privacy Rule guidance states that individuals can get digital copies of digital information (or even digital copies of records kept on paper, as long as the practice has a scanner). Companies are developing tools and services that enable individuals and their care partners to collect, use, and store health records. Request digital (or paper, if that is preferred) copies of blood work, imaging, discharge instructions, and corresponding reports before you leave the practice.
What Happens to Medical Records When Offices Close? The Law
The Health Insurance Portability and Accountability Act (HIPAA) does not require a physician to retain medical records for any particular period of time. (HIPAA covered entities – which include physicians who bill health insurers for care – are required to keep records demonstrating compliance with HIPAA for at least six years – but those records are distinct from medical records. ) However, if the physician still has those medical records – or has placed them in storage for safekeeping – the HIPAA requirements to produce them when a patient requests still apply.
) However, if the physician still has those medical records – or has placed them in storage for safekeeping – the HIPAA requirements to produce them when a patient requests still apply.
State laws typically set medical record retention requirements for physicians and may also require the physician to take particular steps (such as notifying a patient) prior to or upon closure of a practice.
An example of some of these state laws:
During the record retention period, these records are considered to be still “available” and subject to the HIPAA right of access. Consult the medical board or the state medical society in the state where the physician has practiced for further information about physician requirements in the event of closure of a practice. The Medical Board should also have information about how to file a complaint if the physician’s practice has closed without any notice or information about how to obtain records.
Irrespective of legal requirements, the American Academy of Family Physicians recommend that patients be notified by a letter that the office is closing, giving them the opportunity to obtain a copy of their medical records or have records forwarded to a physician of their choosing. The office may post an update on their website or social media page(s), if ones exist or run an ad in the local newspaper. Patients should be notified who will be the custodian of the medical records and their contact information.
Patients should be notified who will be the custodian of the medical records and their contact information.
Sorry! The Office Is Closed
Unfortunately, the reality is that most individuals do not get copies of their medical records throughout their care journey. This leaves patients and carepartners in need of records facing significant uncertainty, stress, and frustration when they unexpectedly find out that their doctor’s office has closed. Here are a number of critical tips to assist patients in gathering their medical records, directly and indirectly, in the event their doctor’s office has closed.
 (As noted above, state laws may allow for them to be destroyed even sooner than 10 years.)
(As noted above, state laws may allow for them to be destroyed even sooner than 10 years.) Social media managers are often very responsive and may be an additional avenue for connecting individuals to the information they need if it is perceived that delays in response may be detrimental to their company’s reputation.
Social media managers are often very responsive and may be an additional avenue for connecting individuals to the information they need if it is perceived that delays in response may be detrimental to their company’s reputation.
 Consequently, the specific state’s county probate court may be contacted to confirm if there is a designated executor of estate that has authority over records retention processes. Alternatively, an obituary may list surviving next of kin which may also be contacted for more information on records retention.
Consequently, the specific state’s county probate court may be contacted to confirm if there is a designated executor of estate that has authority over records retention processes. Alternatively, an obituary may list surviving next of kin which may also be contacted for more information on records retention.

Individuals may also file a complaint with the Office of Civil Rights (OCR) at the Department of Health and Human Services (HHS) if all efforts have been exhausted and the needed medical records have not been obtained.
A closed practice does not need to be a dead end for patient access. Proactively requesting copies of medical records throughout one’s care journey can prevent encountering such patient access barriers. Continuing to share best practices for navigating patient access barriers, from legal, regulatory, and practical standpoints, is in the best interest of all patients.
Grace Cordovano, PhD, BCPA is a board-certified patient advocate specializing in the oncology space, a patient experience enhancer, and information unblocker.
Deven McGraw , JD, MPH, LLM (@healthprivacy) is the Chief Regulatory Officer at Ciitizen (and former official at OCR and ONC). She blogs at ciitizen.com.
She blogs at ciitizen.com.
Aaron Miri is the Chief Information Officer for The University of Texas at Austin comprising of the Dell Medical School, UT Health Austin clinical enterprise, research, and community impact missions.
Spread the love
Categories: Uncategorized
Tagged as: Aaron Miri, Deven McGraw, Grace Cordovano, Health Data, HIPAA, Medical Records
California Health & Safety Code section 123100 et seq. establishes a patient's right to see and receive copies of his or
her medical records, under specific conditions and/or requirements as shown below. The law only addresses the patient's
request for copies of their own medical records and does not cover a patient's request to transfer records between
healthcare providers or to provide the records to an insurance company or an attorney. The request to transfer medical
records is considered a matter of "professional courtesy" and is not covered by law. No statutes cover record transfers
and there is no set protocol for transferring records between providers. Generally, physicians will transfer records
without charging a fee; however, some doctors do charge a fee associated with copying and mailing the paperwork.
Physicians will require a patient to sign a records release form to transfer records.
No statutes cover record transfers
and there is no set protocol for transferring records between providers. Generally, physicians will transfer records
without charging a fee; however, some doctors do charge a fee associated with copying and mailing the paperwork.
Physicians will require a patient to sign a records release form to transfer records.
If you have followed the requirements outlined in the Health & Safety Code and the physician has not complied with your request, you may file a complaint with the Medical Board. Please include a copy of your written request(s). The physician will be contacted to determine the reason for failing to provide you with access to your medical records.
Section 123110 of the Health & Safety Code specifically provides that any adult
patient, or any minor patient who by law can consent to medical treatment (or certain
patient representatives), is entitled to inspect patient records upon written request
to a physician and upon payment of reasonable clerical costs to make such records
available. The physician must then permit the patient to view their records
during business hours within five working days after receipt of the written
request. The patient or patient's representative may be accompanied by one other
person of their choosing. Prior to inspection or copying of records, physicians
may require reasonable verification of identity, so long as this is not used oppressively
or discriminatorily to frustrate or delay compliance with this law.
The physician must then permit the patient to view their records
during business hours within five working days after receipt of the written
request. The patient or patient's representative may be accompanied by one other
person of their choosing. Prior to inspection or copying of records, physicians
may require reasonable verification of identity, so long as this is not used oppressively
or discriminatorily to frustrate or delay compliance with this law.
The patient or patient's representative is entitled to copies of all or any portion
of their records that he or she has a right to inspect, upon written request
to the physician. The physician may charge a fee to defray the cost of copying,
not to exceed 25 cents per page or 50 cents per page for records that are copied
from microfilm, along with reasonable clerical costs. By law, a patient's records
are defined as records relating to the health history, diagnosis, or condition of
a patient, or relating to treatment provided or proposed to be provided to the patient. Physicians must provide patients with copies within 15 days of receipt
of the request.
Physicians must provide patients with copies within 15 days of receipt
of the request.
According to subdivision 123110(d) of the Health and Safety Code, the patient, patient’s representative, or an employee of a nonprofit legal services entity representing the patient is entitled to a copy at no charge of the relevant portion of the patient’s record upon presenting the provider a written request and proof that the records, or supporting forms, are needed to support a claim or appeal regarding eligibility for a public benefit program, a petition for U nonimmigrant status under the Victims of Trafficking and Violence Protection Act, or a self-petition for lawful permanent residency under the Violence Against Women Act. The requestor is entitled to no more than one copy of any relevant portion of their record free of charge. This does not apply to any patient represented by a private attorney who is paying for the costs related to a patient’s claim or appeal, pending the outcome of that claim or appeal. “Private attorney” means any attorney not employed by a non-profit legal services entity. (Health and Safety Code section 123110(d)(3)).
“Private attorney” means any attorney not employed by a non-profit legal services entity. (Health and Safety Code section 123110(d)(3)).
Effective January 2021, Health and Safety Code section 123114 was added establishing that a healthcare provider shall not charge a fee to a patient for filling out forms or providing information responsive to forms that support a claim or appeal regarding eligibility for a public benefit program.
The public health benefit programs include Medi-Cal; the In-Home Supportive Services Program; the California Work Opportunity and Responsibility to Kids (CalWORKS) Program; Social Security Disability Insurance benefits; Supplemental Security Income/State Supplementary Program for the Aged, Blind and Disabled (SSI/SSP) benefits; federal veterans service-connected compensation and nonservice-connected pension disability; CalFresh; the Cash Assistance Program for the Aged, Blind, and Disabled Legal Immigrants; and a government-funded housing subsidy or tenant-based housing assistance program.
Copies of x-rays or tracings from electrocardiography, electroencephalography, or electromyography do not have to be provided to the patient or patient's representative if the originals are transmitted to another health care provider upon written request of the patient and within 15 days of receipt of the request. A patient may request to purchase copies of their x-rays or tracings. All reasonable costs, not exceeding actual costs, may be charged to the patient or patient's representative.
A physician may choose to prepare a detailed summary of the record pursuant to Health
& Safety Code section 123130 rather than allowing access to the entire record. This
summary must be made available to the patient within 10 working days from the date of the
patient's request. If more time is needed, the physician must notify the patient of this
fact and the date that the summary will be completed, not to exceed 30 days between the
request and the delivery of the summary. If the patient specifies to the physician that
he or she is interested only in certain portions of the record, the physician may include
in the summary only that specific information requested. The summary must contain information
for each injury, illness, or episode and any information included in the record relative to:
chief complaint(s), findings from consultations and referrals, diagnosis (where determined),
treatment plan and regimen including medications prescribed, progress of the treatment, prognosis
including significant continuing problems or conditions, pertinent reports of diagnostic procedures
and tests and all discharge summaries, and objective findings from the most recent physician
examination, such as blood pressure, weight, and actual values from routine laboratory tests.
The summary must contain a list of all current medications prescribed, including dosage, and any
sensitivities or allergies to medications recorded by the physician.
If the patient specifies to the physician that
he or she is interested only in certain portions of the record, the physician may include
in the summary only that specific information requested. The summary must contain information
for each injury, illness, or episode and any information included in the record relative to:
chief complaint(s), findings from consultations and referrals, diagnosis (where determined),
treatment plan and regimen including medications prescribed, progress of the treatment, prognosis
including significant continuing problems or conditions, pertinent reports of diagnostic procedures
and tests and all discharge summaries, and objective findings from the most recent physician
examination, such as blood pressure, weight, and actual values from routine laboratory tests.
The summary must contain a list of all current medications prescribed, including dosage, and any
sensitivities or allergies to medications recorded by the physician.
If the patient specifies to the physician that he or she is interested only in certain
portions of the record, the physician may include in the summary only that specific
information requested. The summary must contain information for each injury, illness,
or episode and any information included in the record relative to: chief complaint(s),
findings from consultations and referrals, diagnosis (where determined), treatment
plan and regimen including medications prescribed, progress of the treatment, prognosis
including significant continuing problems or conditions, pertinent reports of diagnostic
procedures and tests and all discharge summaries, and objective findings from the
most recent physician examination, such as blood pressure, weight, and actual values
from routine laboratory tests. The summary must contain a list of all current medications
prescribed, including dosage, and any sensitivities or allergies to medications
recorded by the physician.
There are some exceptions to the absolute requirements shown above: a physician may refuse the request of a minor's representative to inspect or obtain copies of the minor's records if a physician determines that access to the patient records requested by the representative would have a detrimental effect on the physician's professional relationship with the minor patient or the minor's physical safety or psychological well-being.
A physician may refuse a patient's request to see or copy their mental health records if the physician determines there is a substantial risk of significant adverse or detrimental consequences to the patient if such access were permitted, subject to the following conditions:

Events
Today, it is not uncommon for people retiring due to old age to face the problem of confirming work experience. What to do if you encounter this issue.
What to do if you encounter this issue.
The essence of the problem
Until 1990, the procedure for obtaining the information necessary for calculating a pension was simple and understandable. A person contacted the archive or personnel department of the enterprise where he worked, and quickly received comprehensive information. After starting at 9In the 0s of the privatization process, the liquidation of state enterprises, the emergence of commercial structures, the process of obtaining certificates became more complicated, since documents were often lost. Unfortunately, many leaders did not realize the importance of maintaining personnel records. Meanwhile, personnel documents contain important information for assigning a pension to an employee , confirm the length of service, the employee's salary, position (if we are talking about professional categories of citizens eligible for early retirement).
How to confirm the length of service before January 1, 1998
sample. And if all the entries in it are framed correctly, then usually no problems arise.
And if all the entries in it are framed correctly, then usually no problems arise.
In the absence of a work book , as well as if it contains incorrect and inaccurate information or there are no records of individual periods of work, :
- written employment contracts drawn up in accordance with the labor legislation in force on the day of the occurrence of the relevant legal relationship;
- work books of collective farmers;
- certificates issued by employers or relevant state (municipal) bodies;
- extracts from orders;
- personal accounts and payroll statements.
If documents on work are lost due to natural disaster (earthquake, flood, hurricane, fire, etc.) and it is impossible to restore them more witnesses.
In case of loss of work documents due to negligent storage, deliberate destruction and similar reasons through no fault of the employee, periods of work are established based on the testimony of two or more witnesses who know this employee through joint work with one employer and who have documents on his work for the time, in respect of which they confirm the work of a citizen. The nature of the work is not confirmed by the testimony of witnesses!
The nature of the work is not confirmed by the testimony of witnesses!
At the same time, the duration of the length of service established on the basis of witness testimony cannot exceed half of the length of service required for the assignment of an insurance pension .
So for the appointment of an insurance old-age pension on a general basis in 2019, an insurance period of at least 10 years is required. Accordingly, according to testimony, no more than 5 years of insurance experience can be confirmed.
As an example, consider the following life situation:
Question: How can I confirm the work experience at the state farm from 1985 to 1997 if the work book is lost. The state farm was liquidated in the early 2000s, the documents were not handed over to the archive.
Answer: If documents on personnel and payroll records of the state farm are not preserved in the archival institution, the period of work on the state farm can be confirmed by the testimony of two or more colleagues who worked together with him on this state farm between 1985 to 1997. At the same time, the fact of the work of witnesses must be documented, including work books. At the same time, the territorial body of the PFR requests information about the absence (presence) of state farm documents in storage in an archival institution or in the archival department of the municipality.
At the same time, the fact of the work of witnesses must be documented, including work books. At the same time, the territorial body of the PFR requests information about the absence (presence) of state farm documents in storage in an archival institution or in the archival department of the municipality.
For example, the first witness worked at the Iskra state farm in the Dzun-Khemchik district from 09/01/1990 to 04/30/1998, and the second witness worked from 05/01/1987 to 11/30/1994. In this case, the period confirmed by both witnesses, that is, from 01.09..1990 to 11/30/1994 - in total 4 years 03 months 1 day, which will be counted in the insurance period.
The decision to establish periods of work is made on the basis of testimonies given to the body providing pensions at the place of establishment of the pension or at the place of residence of the witness. If a witness is unable to testify for health reasons or other valid reasons, witness testimony certified in accordance with the established procedure may be submitted in writing.
How work periods after January 1, 1998 are confirmed
IMPORTANT! The periods of work of citizens after January 1, 1998 are not confirmed by the testimony of witnesses, since only the periods of work for which insurance premiums were accrued and paid to the Pension Fund are included in the insurance period.
This is due to the fact that in our republic a unified system of personalized registration of insured persons in the system of compulsory pension insurance has been implemented since 1998 years. Since 1998, employers have provided the FIU with information about each employee and the accruals of insurance premiums for the future pension of their employees.
Share news
The purpose of the medical book is to confirm that its owner is not a carrier of infectious diseases and does not pose a threat to others. The document is drawn up by employees of grocery stores and stalls, employees of educational institutions, catering establishments, medical institutions, beauty salons, household utilities (dry cleaners, laundries), etc. The vacancy of a flight attendant or railway conductor also requires the applicant to have a medical book.
The document is drawn up by employees of grocery stores and stalls, employees of educational institutions, catering establishments, medical institutions, beauty salons, household utilities (dry cleaners, laundries), etc. The vacancy of a flight attendant or railway conductor also requires the applicant to have a medical book.
The document is issued by municipal polyclinics and private medical centers. To get a medical book, you need to pass tests and get an appointment with several doctors. The list of specialists and laboratory tests depends on the specialty. Urine and blood tests, the conclusion of a therapist are mandatory for everyone.
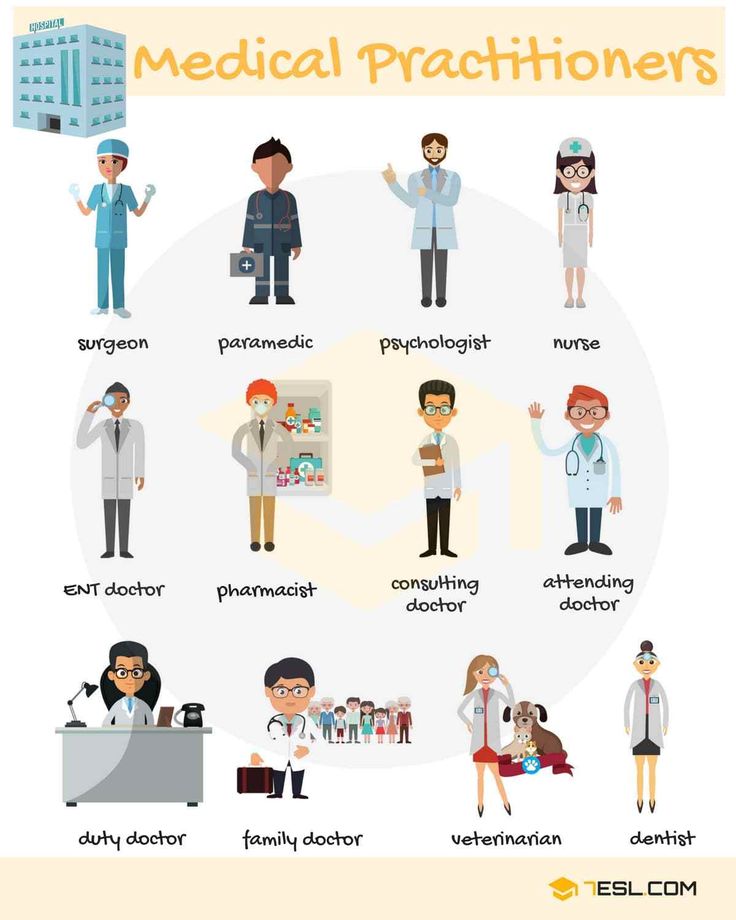
Registration of a document is impossible without the seals of an ENT specialist, surgeon, therapist, neurologist, narcologist and psychiatrist. Women should also get an appointment with a gynecologist. The document is not issued if there are serious vision problems, disorders of the cardiovascular system or psychiatric disorders.
Medical certificate is issued in several cases:
The certificate is valid for 3 years for people under retirement age.
Under the abbreviation is the name of the state inspection, which issues permission to drive yachts, boats, jet skis, motor boats. Medical certificate is issued for a period of 12 months. This means that the owner or captain of a recreational craft is required to undergo an annual survey.
To obtain a certificate, men must visit 7 doctors. Among them are a therapist, ENT, ophthalmologist and others. For women, there is a requirement to visit a gynecologist (total 8 doctors). The conclusions of a psychiatrist and narcologist can only be obtained at the clinic at the place of registration or registration.![]() You need to come to the appointment with the doctor with the results of the EEG. Contacting a private clinic will significantly speed up the process of obtaining a medical certificate.
You need to come to the appointment with the doctor with the results of the EEG. Contacting a private clinic will significantly speed up the process of obtaining a medical certificate.
The right to carry a weapon is granted only to those who have the appropriate license. Its registration is impossible without a medical certificate. The latter certifies that a person does not have mental and other diseases that prevent possession of weapons:
The certificate is valid for six months. During this time, you need to issue a license. The last one is valid for 5 years. The document is drawn up by hunters, security guards, who are supposed to have weapons on duty, as well as any healthy citizen of the country to use weapons in self-defense. To obtain a certificate, you need the conclusions of a narcologist, ophthalmologist, therapist and psychiatrist.
The document is required for employment at enterprises with harmful and difficult working conditions, as well as in the regions of the Far North. In addition, the certificate is issued by applicants for vacancies in the field of transport logistics, catering, food industry, trade, etc.
The procedure for obtaining a document requires visiting a number of specialists and passing tests. Without fail, the applicant for certificate 086y must undergo a test for HIV and AIDS. The document is not issued without the data of a fluorographic examination. The statute of limitations of the latter should not exceed one year. A narcologist and a psychiatrist are visited at a polyclinic at the place of residence or registration. The rest of the specialists can be passed at any medical institution.
Previously, everyone who wanted to visit the pool had to draw up a certificate. Today, this requirement has been preserved only in relation to certain categories of citizens:

To issue a certificate, you need the conclusions of a dermatologist, therapist, venereologist, gynecologist. You can not do without tests that should confirm the absence of infections, including HIV. It is mandatory to give feces for worms and scrapings for enterobiasis. To obtain a certificate, you need up-to-date data from a fluorographic examination (the procedure is no more than a year old).
The document is valid for six months. The certificate is then reissued.
The document certifies that a citizen, for health reasons, can perform official duties and does not pose a threat to others. Schizophrenia, epilepsy, alcohol, drug addiction and other mental disorders are grounds for refusing to issue a certificate.
To obtain a document, you need to take a blood test and get an appointment with a number of specialists with EEG and fluorography data. In 2014, a requirement was introduced to visit a narcologist and psychiatrist at the place of registration. Other doctors can be seen in any medical institution, including private clinics.
Other doctors can be seen in any medical institution, including private clinics.
Attention! The statute of limitations for fluorography should not exceed 1 year.
A health passport is created for every person who issues a medical book or certificate for obtaining a driver's license. It is issued after the first medical examination and is kept by the owner. The passport is provided to doctors at each subsequent medical examination. It contains information about the state of health, test results, recommendations of doctors, as well as the date of the examination.
Do not confuse a health passport with a medical book (specify exactly what the employer requires). In case of loss of the document, you need to contact the medical institution that issued it. You will be provided with a duplicate. Each health passport has an individual number. Only a medical worker has the right to fill out a document.
Pre-trip inspection is a mandatory condition for organizing a working day for all enterprises that have a fleet of vehicles and have a staff of drivers. It does not matter what kind of activity the company is engaged in. A pre-trip inspection is mandatory both for employees of transport companies engaged in freight and passenger transportation, and for enterprises whose drivers serve regular staff. The requirement is designed to ensure the safety of passengers and other road users.
It does not matter what kind of activity the company is engaged in. A pre-trip inspection is mandatory both for employees of transport companies engaged in freight and passenger transportation, and for enterprises whose drivers serve regular staff. The requirement is designed to ensure the safety of passengers and other road users.
The inspection includes measuring the pulse, blood pressure and talking to the driver. If there are signs of intoxication, tests for alcohol are carried out. The right to pre-trip inspection belongs to an organization that has the appropriate license.
The procedure is aimed at protecting the population of Russia from dangerous diseases and epidemics associated with a large flow of migrants into the country. A foreign citizen undergoes a medical examination for the Federal Migration Service in the following cases:
AIDS, syphilis, hepatitis, drug addiction, tuberculosis are the grounds for refusal to stay on the territory of the Russian Federation.