Primary Authors: Jessica Ahn, Vi Dinh; Co-authors: Jade Deschamps, Satchel Genobaga, Annalise Lang, Victor Lee, Reed Krause, Devin Tooma, Seth White. Oversight, Review, and Final Edits by Vi Dinh (POCUS 101 Editor).
An unrecognized or untreated Deep Vein Thrombosis (DVT) in the lower extremities is a major concern because a clot can dislodge and lead to a pulmonary embolism and hemodynamic instability.
Point of Care Compression Ultrasound is a quick and non-invasive way to assess for DVT with very high sensitivity and specificity so you can determine if anticoagulant therapy is necessary (Burnside 2008).
In this post we will show you how to use Point of Care Ultrasound (POCUS) to:
After learning these principles, you will be able to use Point of Care Compression Ultrasound to assess for DVTs in the lower extremities with ease! Below is a Deep Vein Thrombosis Ultrasound PDF Pocket Card you can download to help you remember the most important points.
Table of Contents
Download DVT Ultrasound Card PDF HERE
DVT Ultrasound Pocket Card PDFLike this Post?
Sign Up For POCUS 101 Updates!
 This is a rare complication, but something you should be aware of (Lockhart, Sheldon & Robbin).
This is a rare complication, but something you should be aware of (Lockhart, Sheldon & Robbin). 
The venous anatomy of the lower extremity is fairly simple. Going from proximal to distal, here are the most important veins in the leg you will need to know for DVT ultrasound:
The most proximal vessel is the Common Femoral Vein (CFV), which gives off an important superficial branch known as the great saphenous vein. The CFV continues on to give off a deep femoral vein, and a femoral vein.
Editor’s Note: The Femoral Vein is also previously known as the Superficial Femoral Vein. Don’t be misled by the name – the (superficial) femoral vein is actually part of the deep venous system.
A study from 2011 showed that 75% of junior clinicians believed this vein was a part of the superficial venous system (Thiagarajah, Venkatanarasimha & Freeman). A clot in the (superficial) femoral vein is in fact a deep vein thrombosis and requires anticoagulant therapy to prevent a pulmonary embolus. Don’t get confused by the nomenclature!
As the femoral vein travels inferiorly and medially, it enters into the adductor canal and passes posterior to the knee to become the popliteal vein. At the level of the calf, the popliteal vein gives rise to three other deep veins: the anterior tibial vein, the posterior tibial vein, and the peroneal vein (Zitek, Baydoun & Baird).
Veins of the Lower ExtremityLike this Post?
Sign Up For POCUS 101 Updates!
In this section, we will go over a step-by-step ultrasound approach to evaluate for deep vein thrombosis by visualizing the veins and using venous compression using a standard DVT Ultrasound Protocol.
It is important to note that there are several published protocols using anywhere from a 2-point ultrasound scan to a whole leg scan. We have found a 3-point compression ultrasound protocol to be most feasible while maintaining similar sensitivity and specificity when compared to a whole leg scan (Lee, Lee & Yun). We will focus on performing the 3-Point Ultrasound scan in this post, but here are the differences between the protocols that you may encounter:
2-Point Lower Extremity DVT Ultrasound: compression ultrasound including the femoral vein 1 to 2 cm above and below the saphenofemoral junction and the popliteal vein up to the calf veins confluence.
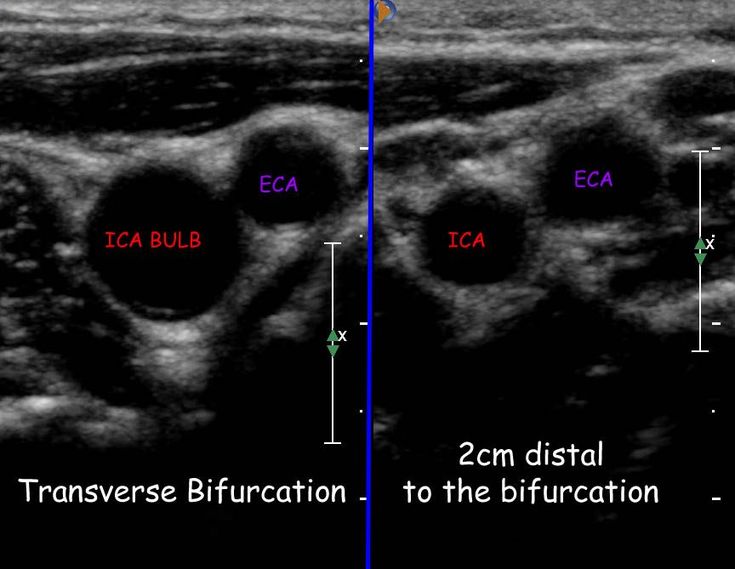
3-Point Lower Extremity DVT Ultrasound: compression ultrasound including the femoral vein 1 to 2 cm above and below the saphenofemoral junction, 1 to 2 cm above and below the bifurcation of the common femoral vein into the deep femoral vein and the (superficial) femoral vein, and lastly the popliteal vein up to the trifurcation into the anterior tibial vein, the posterior tibial vein, and the peroneal vein (Garcia 2018).
Whole Leg/Complete Lower Extremity DVT Ultrasound: involves scanning the leg using compression, color Doppler, and pulse wave Doppler from the common femoral vein all the way to the ankle while evaluating the calf veins.
DVT ProtocolsProper Vein Compression TechniqueOne of the biggest issues with performing DVT ultrasound is knowing how much to compress the vein. If the operator does not apply enough pressure or if the ultrasound probe is not perpendicular, these can lead to false positives for DVTs.
Proper Vein Compression TechniqueYou should apply pressure until the pulsatile artery compresses slightly. If the adjacent vein compresses completely, there is no DVT. Refer to the figure below for an example of proper technique. If the vein does not compress completely, it is likely the patient has a clot in that region.
Editor’s Note: There is a theoretical risk of dislodging a clot and causing a pulmonary embolism with compression. This is a rare complication, but something you should be aware of.
This is a rare complication, but something you should be aware of.
 As the probe moves distally, the artery will typically bifurcate first and then the vein.
As the probe moves distally, the artery will typically bifurcate first and then the vein.

Like this Post?
Sign Up For POCUS 101 Updates!
Deep vein thrombosis can be detected in three ways using point of care ultrasound: direct clot visualization, non-compressibility of vein, and augmentation with Color Doppler.
Direct visualization of the echogenic clot with ultrasound is a definitive way to detect a DVT. Among the indirect ways for diagnosing a DVT, compression ultrasound provides the highest sensitivity and specificity. A study of 220 symptomatic patients scanned for DVT with compression ultrasound yielded a 100% sensitivity and 99% specificity (Lensing et al, 1989). In comparison, augmentation with Color Doppler does not improve the accuracy of scanning and requires squeezing the patient’s leg, which could dislodge any present clots and cause a pulmonary embolism (Lockhart, Sheldon & Robbin; Blaivas et al).
In comparison, augmentation with Color Doppler does not improve the accuracy of scanning and requires squeezing the patient’s leg, which could dislodge any present clots and cause a pulmonary embolism (Lockhart, Sheldon & Robbin; Blaivas et al).
Our recommendation to diagnose DVT is to first use the direct visualization technique. If an echogenic mass is not apparent, we recommend evaluating the compressibility of the veins. The use of color Doppler and augmentation are optional modalities.
Remember to download the DVT Ultrasound Pocket Card PDF as a reference for DVT Ultrasound technique, pathology, and false positives:
Download DVT Ultrasound Pocket Card PDF HERE
DVT Ultrasound Pocket Card PDFDirect Clot Visualization with UltrasoundDepending on the age of a clot, you may see an echogenic mass inside the vessel on ultrasound if your probe is directly over the mass. You may not be able to see acute thrombi because they are anechoic or hypoechoic and they tend to be near the edges of the lumen. As the thrombus ages, it becomes more echogenic and retracts from the vein walls, making it much easier to detect with ultrasound. Therefore, when scanning for clots, do not just rely on direct visualization and always be sure to perform the compression technique to not miss any acute DVTs.
As the thrombus ages, it becomes more echogenic and retracts from the vein walls, making it much easier to detect with ultrasound. Therefore, when scanning for clots, do not just rely on direct visualization and always be sure to perform the compression technique to not miss any acute DVTs.
Examples of Direct Clot Visualization of DVT
DIrect Clot Visualization – DVTEchogenic Mobile Clot – DVTNon-Compressibility with UltrasoundYou can also detect a DVT by compressing the veins. If you apply pressure with the probe until the artery compresses slightly and the vein compresses completely, there is likely no DVT at that spot. However, if you apply enough pressure that the artery compresses but the vein does not compress completely this is considered a “non-compressible” vein and it is likely the patient has a clot in that region.
Examples of Non-Compressible Veins of DVT
Non-compressible Common Femoral Vein and Echogenic ClotNon-compressible Popliteal Vein. Remember, Pop on Top!Non-compressible (Superficial) Femoral VeinAugmentation with Color Doppler
Remember, Pop on Top!Non-compressible (Superficial) Femoral VeinAugmentation with Color DopplerYou can augment venous flow by squeezing the leg distal to where you are scanning. If Color Doppler demonstrates a homogenous increase in venous flow, this suggests that there is no occlusive thrombus between where you are squeezing and scanning. However, if there is no increase in venous flow, there could be a DVT.
Editor’s Note: Use this method with caution as there could be a risk of dislodging any existing clots and causing a pulmonary embolism.
Obstructed Veins with Color Doppler of DVT
Clot in Great Saphenous Vein reduced Color Doppler flowObstructed (Superficial) Femoral Vein with no flow on Color DopplerVideo Summary for DVT UltrasoundBelow is a video we made summarizing how to obtain the views for DVT ultrasound as well as how to evaluate for DVT pathology:
Deep Vein Thrombosis TreatmentIt is important to treat DVT since one out of three patients with untreated DVT experience clinically significant pulmonary embolism, and the short-term mortality rate from untreated PE can exceed 20% (Burnside et al).
It is beyond the scope of this post to explain all of the possible treatments for DVT, but here is a proposed algorithm adapted from Mazzolai 2017:
DVT Management AlgorithmLike this Post?
Sign Up For POCUS 101 Updates!
There are a few structures that can be mistaken for a deep vein thrombosis because they look like non-compressible vessels. These include superficial thrombophlebitis, Baker’s cysts, lymph nodes, pseudoaneurysms, and groin hematomas, which we will show below.
To help avoid these false positives, be sure to always identify that the vein is next to an artery. Additionally, if you compare the vein in Short Axis and Long Axis views, it will look circular in the short axis view and cylindrical in the long axis view.
Circular Vein in Short Axis ViewCylindrical Vein in Long Axis ViewSuperficial ThrombophlebitisSuperficial thrombophlebitis occurs when there is a clot in a superficial vein, like the great and small saphenous veins and the varicose veins.
A clot in a superficial vein will show the same signs on ultrasound as in a deep vein; you can see an echogenic mass with direct visualization, non-compressibility, and decreased or absent color flow. The major difference is that superficial veins do NOT accompany arteries while deep veins do (Naringrekar et al).
This pitfall is more likely in obese patients whose superficial veins are enlarged and can be mistaken as deep veins.
Superficial Thrombophlebitis (Nasr et al). Baker’s Cyst
Baker’s CystA Baker’s cyst is a fluid-filled cyst in the popliteal bursa on the back of the knee. This can result from inflammation of the knee joint or a knee injury, like a cartilage tear.
These popliteal cysts can present with similar symptoms as a deep vein thrombosis such as sharp knee pain, calf swelling, and occasionally erythema.
On ultrasound, a Baker’s cyst appears as a circular anechoic mass with sharply defined borders in both the longitudinal and transverse view (Zitek, Baydoun & Baird). On Color Doppler, there should be no flow.
Baker’s Cyst IllustrationBaker’s Cyst on Ultrasound (Naringrekar et al)Lymph NodesLymph nodes are part of the adaptive immune system and can become inflamed when the body is fighting an infection.
On ultrasound, a lymph node can look similar to a clot because it is a hypoechoic oval structure with a hyperechoic center. However, if you scan the lymph node in the longitudinal view, it becomes apparent that the object is circumscribed and not tubular in structure like a vein (Zitek, Baydoun & Baird). Lastly, a lymph node will disappear quickly if you attempt to trace it up and down, unlike an artery or vein that will be continuous structure.
Lastly, a lymph node will disappear quickly if you attempt to trace it up and down, unlike an artery or vein that will be continuous structure.
A pseudoaneurysm occurs when there is a partial rupture of an artery wall that leads to an outpouching of the artery with the accumulation of periarterial blood. This most commonly occurs from arterial trauma from an interventional medical procedure, gunshot, or a stab wound (Montorfano et al). These sites can become infected and give off emboli.
On ultrasound, pseudoaneurysms present as anechoic or hypoechoic images, sometimes with moving echoes. With Color Doppler, you can see a “Yin-Yang Sign” from the circular motion of blood inside the pseudoaneurysm cavity. In systole, blood flows towards the pseudoaneurysm cavity (red) while in diastole the blood moves back towards the arterial lumen (blue)(Montorfano et al).
A groin hematoma occurs when blood leaks from an artery, typically the femoral artery, and causes localized swelling. Some risk factors can include recent procedure in that area, obesity, anticoagulation, and peripheral vascular disease (Kosmidou & Karmpaliotis).
On ultrasound, a groin hematoma will be hypoechoic with some anechoic areas scattered throughout. If you scan the hematoma in the longitudinal view, it becomes obvious that the object is circumscribed and not tubular like a vein or artery.
Groin Hematoma (Ony et al).References , Brown, M., Kline, J. (2008). Systematic review of emergency physician-performed ultrasonography for lower-extremity deep vein thrombosis. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine 15(6), 493-8. https://dx.doi.org/10.1111/j.1553-2712.2008.00101.x
, Brown, M., Kline, J. (2008). Systematic review of emergency physician-performed ultrasonography for lower-extremity deep vein thrombosis. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine 15(6), 493-8. https://dx.doi.org/10.1111/j.1553-2712.2008.00101.x doi.org/10.1016/b978-1-4160-3773-6.10023-0
doi.org/10.1016/b978-1-4160-3773-6.10023-0
 91
91 , Doris, C., McGrath, F., Cogo, A., Sabine, M., Ginsberg, J., Prandoni, P., Turpie, A., Hirsh, J. (1997). A Comparison of Compression Ultrasound With Color Doppler Ultrasound for the Diagnosis of Symptomless Postoperative Deep Vein Thrombosis. Archives of Internal Medicine 157(7), 765.
, Doris, C., McGrath, F., Cogo, A., Sabine, M., Ginsberg, J., Prandoni, P., Turpie, A., Hirsh, J. (1997). A Comparison of Compression Ultrasound With Color Doppler Ultrasound for the Diagnosis of Symptomless Postoperative Deep Vein Thrombosis. Archives of Internal Medicine 157(7), 765.Normal venous flow and valve movement,
NORMAL FLOW
In the normal cicumstance, the superficial system drains the subcutaneous tissues and periodically empties into the deep system via perforating veins.
Flow direction should always be:
Incompetent valve & perforator leading to venous reflux.
INCOMPETENT FLOW
With distal augmentation, flow initially goes cephalad. It then refluxes back down the leg through the malfunctioning valve.
An incompetent perforating vein also allows blood to flow from the deep veins to the surface veins.
This combination of back pressure causes dilation and tortuosity of the veins (ie varicosites).
Normal venous valve.
ultrasound of a competent vein valve
Normal competent venous valve as seen on b mode ultrasound. It is important not to mistake this for thrombus.
Ultrasound of a competent valve transverse view
The 2 valve leaflets can be seen meeting in this transverse cross-sectional ultrasound view of the vein. This represents a competent valve however doppler assessment would be required to confirm this.
Incompetent vein B mode ultrasound
This swirling slow moving blood is typically seen in veins when using high frequency ultrasound. Colour doppler is unlikely to demonstrate flow due to the very slow velocity not creating a doppler shift within the range of the probe. The to-fro nature of the flow indicates incompetence.
ultrasound mobile superficial thrombosis
Superficial thrombophlebitis on ultrasound. The non-occlusive mobile thrombus is visible inside the vein. There is increase echogenicity of the subcutaneous fat surrounding the vein consistant with fovcal inflammation (phlebitis).
The non-occlusive mobile thrombus is visible inside the vein. There is increase echogenicity of the subcutaneous fat surrounding the vein consistant with fovcal inflammation (phlebitis).
ultrasound mobile superficial thrombo-phlebitis
Superficial thrombophlebitis ultrasound
Leg Vein Anatomy
REF: Journal Of Vascular Surgery, Special Communication, 2005. (215kB PDF file)
We recommend reviewing this thorough document.
Importantly, to avoid confusion, the ‘Long Saphenous’ is now the ‘Great Saphenous’.
Below is a basic outline of the anatomy and function of the veins and what constitutes venous incompetence. Be aware however that there are numerous anatomical variations.
Valves
The veins contain a series of valves along their course, preventing retrograde flow back down the leg. These valves operate like two plastic doors opening up the leg. If back pressure is applied, they swing closed, pushing against each other, blocking reverse flow down the leg.
If back pressure is applied, they swing closed, pushing against each other, blocking reverse flow down the leg.
If functioning normally, it is a competent valve. If blood is able to pass backwards though the valve, it is deemed incompetent.
Depending on the extent of incompetence, this backflow will dilate the supple superficial veins making them tortuous and dilated(varicose veins).
Causes include:
Familial factors with ‘lax’ veins. These distend slightly allowing the valve leaflets to no longer oppose each other.
Injury or thrombosis. Both of these can lead to adherance of valve leaflets to the vein wall, rendering the valve useless.
The Deep Veins
Are the primary route for returning blood to the heart. They collect the venous blood from all the draining muscular and superficial veins.
In the lower limb the deep veins are: (from groin to ankle)

The Superficial Veins
There are 2 main superficial veins draining the subcutaneous tissue of the lower leg:
The Great Saphenous vein (GSV) runs from the medial malleolus, up the medial aspect of the leg, draining into the CFV at the groin as the Sapheno-femoral junction (SFJ).
The Short Saphenous vein (SSV) runs up the posterior midline of the calf. It may drain into the proximal POPV above the knee crease as the Sapheno-Popliteal junction (SPJ). Commonly however, it may continue up the posterior thigh as the Giacomini vein. This will terminate either into the mid/distal SFV or ascend to drain into the proximal LSV.
Incompetence of the SFJ and SPJ are the two primary sources of varicose veins.

Sapheno-femoral Junction Anatomy
Sapheno-Femoral Junction Anatomy
Deep Veins
Superficial Veins:
Sapheno-popliteal (SPJ) anatomy diagram.
The Sapheno-Popliteal Junction
Determine competency and the relationship to the knee crease.
The junction is commonly into the lateral aspect of the popliteal vein.
Common variations are:
Diagram of transverse calf showing the ‘eye-like’ fascia containing the SSV.
The Short Saphenous Vein may terminate in the Giacomini vein with no Sapheno-popliteal junction.
Alternatively it may divide, with a normal SPJ and a Giacomini vein (as in this case).
NOTE: A comprehensive thorough scan can take an hour to complete.
 Some patient will have difficulty with this.
Some patient will have difficulty with this.
Post thromotic syndrome in patients with a past history of DVT can lead to deep venous incompetence. Deep venous incompetence or current DVT is important to exclude as a cause for the patients symptoms.
Deep venous incompetence or current DVT is important to exclude as a cause for the patients symptoms.
Sometimes referred to as the Long Saphenous vein (LSV).

A perforating vein joins the superficial veins to the deep veins. By definition a perforating vein must breech the fascia between the superficial fat and the muscle fascia.
In transverse, scan in a methodical patternup and down the medial calf. Begin with the toe of the probe on the Tibia and do vertical sweeps until you reach the SSV.
Flow should always be superficial to deep (competent).
If flow is observed deep to superficial, the vein is incompetent. Any incompetent perforating veins (IPVs) or competent perforators >3mm should be noted in the report.
Common Perforators The most common perforating veins are shown. |
A CVI study should include the following minimum images:
Ultrasound is used to diagnose diseases in the early stages of development. Ultrasound is safe. The patient does not feel pain. Diagnosis is carried out both in children from birth and in adults. Ultrasound is done according to the prescription of the attending physician. This is a common technology. In Bryansk, examinations are available in almost all polyclinics, private clinics and inpatient hospitals. Diagnostics is inexpensive.
Ultrasound is done according to the prescription of the attending physician. This is a common technology. In Bryansk, examinations are available in almost all polyclinics, private clinics and inpatient hospitals. Diagnostics is inexpensive.
When is an ultrasound indicated?
Ultrasound examination is prescribed by doctors of various fields: gynecologists, cardiologists, ophthalmologists, pulmonologists, phlebologists, neurologists, endocrinologists, surgeons, pediatricians. The doctor may refer you for a standard or special study.
- For the study of bone tissue, densitometry is performed.
- To identify the pathology of blood vessels - Dopplerography.
- Pregnant women are prescribed 3D ultrasound to better monitor the development of the fetus.
An ultrasound examination of the thyroid gland is prescribed for a sharp change in weight, unstable emotional state, severe fatigue, increased drowsiness. The thyroid gland is examined when diabetes mellitus is detected, after taking hormonal drugs. In Bryansk, ultrasound is done in all medical institutions and diagnostic centers.
In Bryansk, ultrasound is done in all medical institutions and diagnostic centers.
If chest pains appear, lymph nodes increase, then the mammologist can refer the patient to an ultrasound of the breast. Gynecologists use ultrasound to determine the development of lactation in women who are breastfeeding. Diagnostics can reveal a tumor, mastopathy, papilloma, cyst at an early stage. It allows you to quickly start treatment in order to avoid complex diseases.
When changes occur in the joints, ultrasound is prescribed. With its help, pathologies in the articular bag, muscles, tendons are determined. In some cases, ultrasound is used in the conduct of a surgical operation.
Where to get an ultrasound in Bryansk?
Many companies offer ultrasound services. On their websites, they indicate the type of diagnosis, the area of research. In private clinics in Bryansk, ultrasound is paid. Government offices and hospitals usually do not require a doctor's fee.
TOP centers in Bryansk by regions
Bezhitsky: Spectrum Diagnostics, Ethel, Romed, Family Clinic; Soviet: Ethel, Es Class Clinic, Ethel, TRK Clinic; Volodarsky: Hospital No. 2, Hemotest; Medica plus; Medsi; MRI Center. Fokinsky: Academy of Health, Tomography Center, My Doctor, MedExpress, Family Clinic.
The price of the service in private clinics depends on the scope of the study. On the websites of companies you can find a price list with the type of ultrasound and its cost.
Login
Via social media:
Or via form:
Email or username
Enter your email address or username.
Password
Enter the password that accompanies your email address.
An ATV, unlike a snowmobile, is an all-weather vehicle. But in order for the all-terrain vehicle to faithfully plow the virgin snow all winter, it must be prepared for operation in the cold season. Otherwise, by the end of winter, or even earlier, the quadric can easily “die”. The AvtoVzglyad portal tells about the nuances of the winter use of "quadrics".
But in order for the all-terrain vehicle to faithfully plow the virgin snow all winter, it must be prepared for operation in the cold season. Otherwise, by the end of winter, or even earlier, the quadric can easily “die”. The AvtoVzglyad portal tells about the nuances of the winter use of "quadrics".
Maxim Stroker
Most often, ATV owners face the problem of difficult starting in cold weather. Perhaps the problem may be in poor contact between the power wires and the battery terminals. If there is oxidation in the connection, then the battery itself does not charge well and at the time of starting in the cold it simply does not have enough voltage to confidently turn the crankshaft with the starter.
The problem is solved simply: disconnect the wires from the battery, remove oxides with sandpaper, and so that they do not form in the future, we process the battery terminals with a special Liqui Moly Kontaktreinig contact cleaner. This combined action aerosol formulation removes metal oxides and grease in a single process. The special chemical formula almost instantly loosens and eliminates oxide salts, restores electrical conductivity, and also blocks leakage currents.
The special chemical formula almost instantly loosens and eliminates oxide salts, restores electrical conductivity, and also blocks leakage currents.
But much more often the cause of difficult starting in cold weather is engine oil. Most ATVs run on 10W-40 or 10W-50 lube during the summer. In general, such oil is considered to be quite all-weather, but if your “quad” is not in a heated garage, but on the street, then in severe frosts, difficulties arise with starting the engine, since the thickened oil provides excessive resistance.
But even if the engine starts, then the first seconds after starting it can work, which is called dry, since it will be very difficult for the oil pump to create the necessary pressure due to the thickened lubricant and supply it to the rubbing surfaces. This is especially dangerous for motors assembled on so-called plain bearings, because due to oil starvation, main or connecting rod bearings can turn.
In order not to encounter such a problem, before the onset of severe cold, you should fill the ATV engine with oil with a viscosity of 5W-50. The Liqui Moly product line has a quality lubricant with the right characteristics, one hundred percent suitable for ATV operation in winter. Liqui Moly ATV 4T Motoroil 5W-50 HC-synthetic motor oil provides maximum performance and engine protection under all operating conditions.
The Liqui Moly product line has a quality lubricant with the right characteristics, one hundred percent suitable for ATV operation in winter. Liqui Moly ATV 4T Motoroil 5W-50 HC-synthetic motor oil provides maximum performance and engine protection under all operating conditions.
Anti-wear additive package and base stock provide maximum ATV engine protection and trouble-free operation over a wide range of temperatures and loads. The oil guarantees easy start-up at low temperatures and high viscosity-temperature stability.
It is by no means superfluous to change the oil in the ATV gearboxes before winter. Despite the fact that there is no winter transmission for ATVs as such, it is still necessary to change the oil before frosts, because water from autumn puddles could well get into these nodes, through a breather or seals, which, mixed with oil, turns into an emulsion . And if you take into account that the gearboxes of modern ATVs have an electrician (someone has an electromagnetic clutch, someone has a servo drive), then there will be continuous problems from such a “slurry” in winter.
If there is any chance that the gearboxes of your "rogue" have taken a sip of water, then in addition to filling in new oil, they also need to be washed. Drain the waste from the gearboxes, tighten the bottom plug, and pour the quick cleaner Liqui Moly Schnell-Reiniger through the filler.
This agent is absolutely safe for electrics and rubber seals of the gearbox, but at the same time it will effectively clean the inside of the assembly from the remnants of the emulsion. For best results, jack up the quad axle you are flushing and turn the wheels forward/back by hand to flush the remaining emulsion from the sidewalls as well. After that, unscrew the drain plug, get rid of the dirty contents and, screwing the plug back, pour in fresh gear oil.
ATVs most often use a transmission with a viscosity of 75W90. It is suitable for most ATVs and is poured into both front and rear gearboxes. The German brand Liqui Moly has in its assortment a synthetic gear oil for motorbike Gear Oil 75W-90.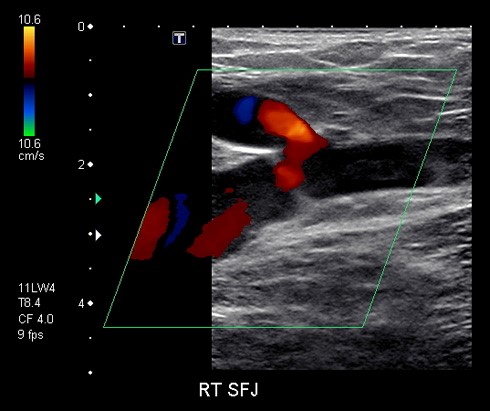 It is in a sense universal, all-weather, and equally suitable for transmissions and motorcycles, and scooters, and ATVs, and snowmobiles.
It is in a sense universal, all-weather, and equally suitable for transmissions and motorcycles, and scooters, and ATVs, and snowmobiles.
This oil contains polyalphaolefins and special additives, due to which the lubricant does not change its properties either at sub-zero or positive temperatures. Its thermo-oxidative stability and resistance to aging allow for extended drain intervals that are significantly higher than other similar oils of similar viscosity.
In any case, check the manufacturer's recommendations before filling gears with oil, as some ATV models require gear oil for clutch operation. By the way, Liqui Moly also has such oils in its product line.
For the running gear to work well, it also needs to be prepared for winter. Namely, lubricate the bushings of the fists and suspension arms with grease with a low freezing point, which at the same time is capable of operating in combined metal-plastic pairs.