It's common to feel tired, or even exhausted, during pregnancy, especially in the first 12 weeks.
Hormonal changes at this time can make you feel tired, nauseous and emotional. The only answer is to rest as much as possible.
Make time to sit with your feet up during the day, and accept any offers of help from colleagues and family.
Being tired and run-down can make you feel low. Try to look after your physical health – make sure you eat a healthy diet, and get plenty of rest and sleep.
Later in pregnancy, you may feel tired because of the extra weight you're carrying. Make sure you get plenty of rest.
As your bump gets bigger, it can be difficult to get a good night's sleep. You might find that lying down is uncomfortable or that you need to use the loo a lot.
Feeling tired will not harm you or your baby, but it can make life feel more difficult, especially in the early days before you've told people about your pregnancy.
You may have strange dreams or nightmares about the baby, and about labour and birth. This is normal.
Talking about them with your partner or midwife can help. Remember, just because you dream something, it does not mean it's going to happen. Relaxation and breathing techniques may be helpful in reducing any anxiety you might be feeling.
The safest position to go to sleep is on your side, either left or right. Research suggests that, after 28 weeks, falling asleep on your back can double the risk of stillbirth. This may be to do with the flow of blood and oxygen to the baby.
Do not worry if you wake up on your back – the research looked at the position pregnant people fell asleep in, as this is the position we keep for longest. If you wake up on your back, you can just turn over and go to sleep again on your side.
You can try supporting your bump with pillows and putting a pillow between your knees.
The baby charity Tommy's has a video about safer sleeping in pregnancy.
Try not to let it bother you if you cannot sleep, and do not worry that it will harm your baby – it will not. If you can, nap during the day and get some early nights during the week.
Avoid tea, coffee or cola drinks in the evening, as the caffeine can make it harder to go to sleep.
Try to relax before bedtime so you're not wide awake. Relaxation techniques may also help, ask your midwife for advice. Your antenatal classes may teach you some techniques, or you could use a pregnancy relaxion CD or DVD.
You could join an antenatal yoga or pilates class. Make sure the instructor knows you're pregnant. Exercise can help you feel less tired, so try to do some activity, such as a walk at lunchtime or going swimming, even if you feel tired during the day.
If lack of sleep is bothering you, talk to your partner, a friend, doctor or midwife.
Read about preventing insomnia, including daytime habits, such as exercising, and bedtime habits, such as avoiding caffeine.
Occasionally, sleeplessness – when accompanied by other symptoms – can be a sign of depression. If you have any of the other symptoms of depression, such as feeling hopeless and losing interest in the things you used to enjoy, speak to your doctor or midwife. There is treatment that can help.
Read about mental health in pregnancy.
Healthtalk.org has videos and written articles of people talking about their symptoms and feelings in the early weeks of pregnancy, including tiredness.
In this video, a midwife explains the various ways pregnant mothers can get more comfortable at night.
Media last reviewed: 25 January 2023
Media review due: 25 January 2026
Pregnancy is all about changes, and some are more dramatic than others. Along with all the physical changes happening to your body, you may also be experiencing symptoms like mood swings, swelling, nausea or morning sickness, to name a few. So, it can be easy to overlook something as straightforward as fatigue.
Along with all the physical changes happening to your body, you may also be experiencing symptoms like mood swings, swelling, nausea or morning sickness, to name a few. So, it can be easy to overlook something as straightforward as fatigue.
But as you may be finding out, fatigue can be quite a challenge, too. Below, we cover everything you can expect from this common pregnancy symptom, its causes, and what you can do to manage it.
Fatigue is totally normal during pregnancy, but people’s experiences with it can vary widely. It may be that you don’t experience much fatigue at all, or it may be that you feel extreme tiredness in early pregnancy that drops off later on. No matter how it affects you, fatigue can generally be characterized by:
Pregnancy fatigue can start as soon as one week after conception, which means it may be an early sign of pregnancy before a test can tell you for sure. It’s also common to start feeling tired any time during the first 12 weeks.
It’s also common to start feeling tired any time during the first 12 weeks.
There are various factors that can cause fatigue, but they differ from trimester to trimester.
The overall cause of fatigue in early pregnancy is simple – your body is preparing for the months ahead. But there are a couple parts of this preparation that can really contribute to feelings of fatigue:
In the second trimester, people typically find that they have more energy – you may be used to the new hormone levels in your body, and your baby isn’t very big yet.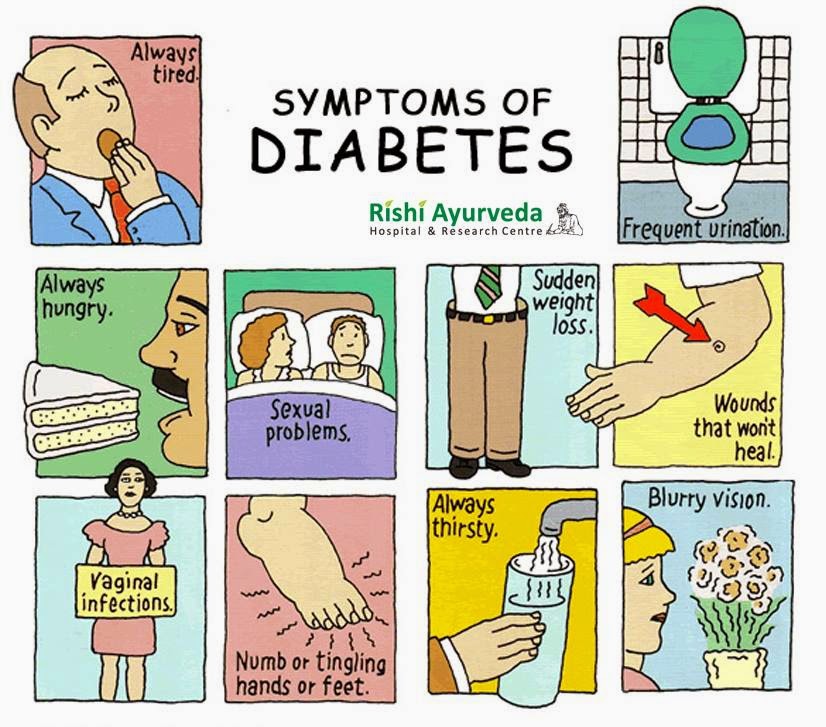 But it’s still possible to feel fatigued in the second trimester, especially if your sleep gets interrupted by pregnancy symptoms like frequent urination and leg cramps.
But it’s still possible to feel fatigued in the second trimester, especially if your sleep gets interrupted by pregnancy symptoms like frequent urination and leg cramps.
When fatigue happens in the third trimester, it’s generally because the baby’s gotten bigger. Carrying around that extra weight can be tiring on its own, but it also makes other things harder, including sleeping comfortably. Plus, as the baby settles into the pelvis, it puts more pressure on the bladder, so nighttime trips to the bathroom may become even more common. And all of that is in addition to any other pregnancy symptoms you’re experiencing.
When it comes to managing fatigue, the best thing you can do is take steps to increase your energy levels. This means:
A solid pregnancy diet can be a great way to keep your energy up. In particular, focus on getting enough iron, which supports red blood cell production and prevents any additional tiredness from anemia (a condition which results from not having enough red blood cells to carry the amount of oxygen your body needs). Foods that are high in protein are also good choices, as protein is a longer-lasting source of energy compared to carbohydrates.
Foods that are high in protein are also good choices, as protein is a longer-lasting source of energy compared to carbohydrates.
You may benefit from eating smaller meals throughout the day. This can help keep your blood sugar and energy levels consistent. It’s also important to drink plenty of water, as water helps your body function properly.
The American College of Obstetricians and Gynecologists recommends that you get at least 150 minutes of moderate aerobic activity each week while you’re pregnant. That may sound like a lot, but if you break it down into 30 minutes of pregnancy-safe exercises per day, it adds up quickly.
Exercise improves blood circulation, which helps bring oxygen to every part of your body. This can give a boost to overall energy levels. Plus, exercise helps manage other pregnancy symptoms like back pain and constipation.
Even if you’re doing everything you can to boost your energy levels, you still have to listen to your body. And when your body is fatigued, rest is the answer. Take breaks throughout the day, nap when you need to and sleep as much as possible. It may help to go to bed earlier, and avoiding fluids for a few hours before going to bed can help cut down on bathroom visits at night.
And when your body is fatigued, rest is the answer. Take breaks throughout the day, nap when you need to and sleep as much as possible. It may help to go to bed earlier, and avoiding fluids for a few hours before going to bed can help cut down on bathroom visits at night.
Fatigue is very common and normal during pregnancy. Still, don’t hesitate to talk to your care provider at any point along your prenatal appointment timeline if you have questions or concerns about your level of tiredness.
But keep in mind, there are times when fatigue may be a symptom of a pregnancy complication like anemia, depression or gestational diabetes. Call your care provider if you experience sudden fatigue, fatigue that completely stops you from doing your daily tasks or if you have fatigue with any of the following:
Whether your pregnancy is making you tired, nauseous or anything else, a prenatal appointment can help. In addition to making sure you and your little one are safe and healthy, your care provider can give you tips and recommendations for every part of your pregnancy.
In addition to making sure you and your little one are safe and healthy, your care provider can give you tips and recommendations for every part of your pregnancy.
Nausea, chest pain, appetite for pickled cucumbers - all this is the action of hormones. During pregnancy, you are under their strong influence.
How do they work? Until you became pregnant, most of the hormones in your body were produced by endocrine glands such as the thyroid gland. Now, many of them also form in the placenta, which is inside the uterus. Immediately after the birth of the baby, the placenta is excreted from the body and pregnancy hormones are no longer needed.
The culprit is human chorionic gonadotropin , which is produced by the embryo and then by the placenta. It is the presence of this hormone in the urine that leads to a positive pregnancy test result. In addition, human chorionic gonadotropin increases the production of another hormone, progesterone , and stops the menstrual cycle.
In addition, human chorionic gonadotropin increases the production of another hormone, progesterone , and stops the menstrual cycle.
Endorphins - These hormones are your biggest allies. These are natural painkillers and calming hormones. They work like morphine. They are called happiness hormones because they are the reason you expect a baby with joy, regardless of nausea and other pregnancy ailments. The source of endorphins is in the brain, where they are produced until the end of labor. The highest concentration of endorphins at the time of childbirth. Thanks to them, the pain becomes weaker, and the stress associated with childbirth is not so tiring. After childbirth, the level of endorphins drops sharply. This is probably the cause of a mild form of postpartum depression.
Estrogens , which affect your sex drive, are first produced by the ovaries and then by the placenta.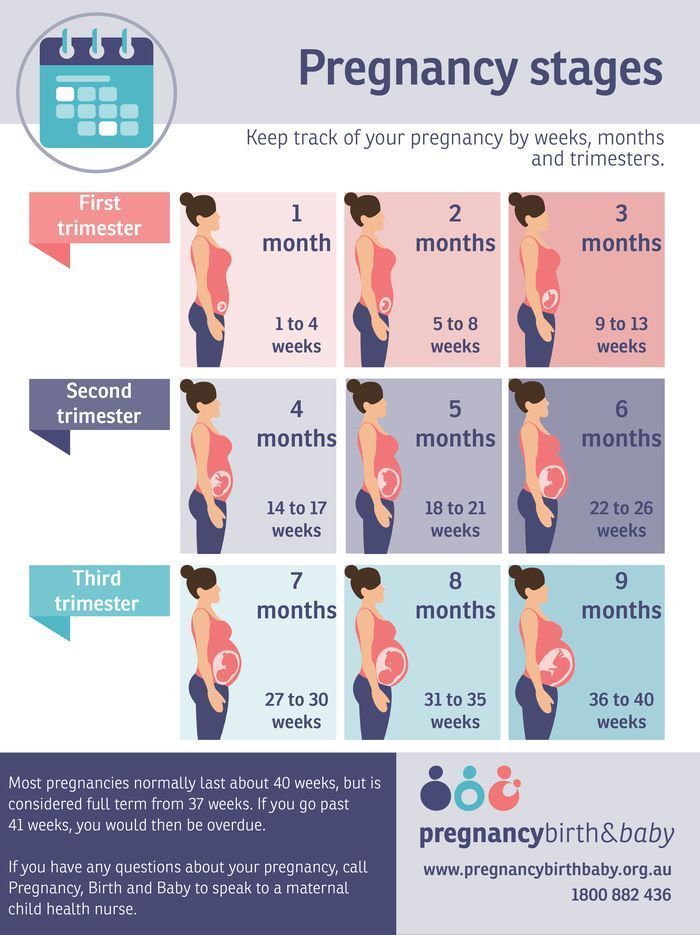 Estrogen production rises rapidly at the beginning of pregnancy. Thanks to estrogen, you feel that the desire for intimacy in the first trimester of pregnancy increases. Estrogens increase the blood supply to the breasts, vagina, vulva, and clitoris, which become especially sensitive. This is interesting! Thanks to pregnancy hormones, sex in the second trimester of pregnancy can be the best in a lifetime, according to scientists!
Estrogen production rises rapidly at the beginning of pregnancy. Thanks to estrogen, you feel that the desire for intimacy in the first trimester of pregnancy increases. Estrogens increase the blood supply to the breasts, vagina, vulva, and clitoris, which become especially sensitive. This is interesting! Thanks to pregnancy hormones, sex in the second trimester of pregnancy can be the best in a lifetime, according to scientists!
They relax muscles and prevent spasms. This is the influence of one of the most important pregnancy hormones: progesterone . Before pregnancy, it was produced, like estrogens, by the ovaries, now this function has passed to the placenta. Progesterone is responsible for most of the changes in your body during pregnancy (including fever, increased breathing). It relaxes the smooth muscles of the uterus and protects against miscarriage.
Preparing for childbirth is the merit of relaxin . Under its influence, the joints of the pelvic bones relax, soften the cervix and increase the elasticity of the surrounding ligaments, so that your uterus will grow, and your child will be able to pass through the birth canal.
Under its influence, the joints of the pelvic bones relax, soften the cervix and increase the elasticity of the surrounding ligaments, so that your uterus will grow, and your child will be able to pass through the birth canal.
Prostaglandins and oxytocin are the hormones that most support the final stages of pregnancy. The rising level of oxytocin is responsible for the development of the maternal instinct. In the last trimester, you begin to feel uterine contractions stimulated by prostaglandins. If you have sex, you can speed up labor because prostaglandins are also found in male semen. Oxytocin stimulates predictive uterine contractions or Braxton-Hicks contractions and then the corresponding labor contractions. In some situations, it stimulates labor and accelerates the passage of the placenta.
Two more hormones, prolactin and placental lactogen , will allow you to breastfeed your baby. Thanks to them, the breasts begin to secrete colostrum (the first very nutritious food that can be excreted as early as the 19th week of pregnancy). Your body will produce it within days of giving birth. Later, milk will appear due to these hormones.
Thanks to them, the breasts begin to secrete colostrum (the first very nutritious food that can be excreted as early as the 19th week of pregnancy). Your body will produce it within days of giving birth. Later, milk will appear due to these hormones.
Pregnancy hormones also affect your appearance:
During your pregnancy, Kätlin Wachtel will supervise and instruct you, working closely with Dr. Marek Scheus. At the end of each room, the time of the next visit will be agreed. You can come to the appointment and ultrasound together with a family member or loved one
Marek Scheus. At the end of each room, the time of the next visit will be agreed. You can come to the appointment and ultrasound together with a family member or loved one
Pregnancy is determined by a gynecologist who, using vaginal ultrasound, determines the duration of pregnancy and childbirth. In addition, the viability of the fetus and the presence of a double pregnancy are assessed. The gynecologist introduces the plan for monitoring pregnant women at the Fetal Ultrasound Center and gives a complete overview of the screenings of the first half of pregnancy, as well as advice on the need for folic acid.
A gynecologist performs a vaginal ultrasound to assess life-threatening malformations and fetal growth dynamics. Ultrasound also evaluates the absence of contraindications for non-invasive prenatal tests (NIPT) to detect chromosomal disorders. The gynecologist takes tests from the cervix.
The gynecologist takes tests from the cervix.
After consultation with a gynecologist, a midwife or nurse will take a blood test from you to screen for fetal chromosomal disorders (Panorama test, PanoramaXP test, Vistara test, Horizon test) and early detection of intrauterine infections (cytomegalovirus infection, toxoplasmosis). If you do not have insurance, you can obtain a certificate for applying for insurance from the Estonian Health Insurance Fund.
Your midwife or nurse will take your pregnancy test, which is best taken on an empty stomach and in the morning between 8:00 and 11:30. It is very important that you remember to take your morning urine test with you.
During the same appointment, your body weight and blood pressure are measured, and a detailed pregnancy history is taken for the OSCAR test. If you have not previously been diagnosed with high blood pressure, but your blood pressure readings are higher than normal several times during your appointment, 24-hour home blood pressure monitoring will be performed with your consent to obtain an objective blood pressure reading.
If necessary, you will be consulted about ailments in the first half of pregnancy (fatigue, nausea, constipation), and if you have a negative Rh factor, the father of your child will be asked to determine the Rh affiliation from his venous blood.
A gynecologist and nurse perform a detailed OSCAR test that assesses the child's risk of chromosomal disorders and the risk of pre-eclampsia, stunting and preterm birth, and also checks the child's early development to identify possible abnormalities that can be assessed at this stage of pregnancy. After the OSCAR test, the gynecologist will explain to you in detail the significance of the test results for the course of your pregnancy and will draw up an individual pregnancy plan for you (pregnancy monitoring plan, possible risks of pregnancy, chronic diseases and continued daily medication, referral to a specialist doctor).
After the OSCAR test, the midwife will register your pregnancy at the Fetal Ultrasound Center. During the appointment, you are advised on the results of the tests performed, a pregnant woman's card is filled in, which indicates the expected date of delivery and the exit on maternity leave.
During the appointment, you are advised on the results of the tests performed, a pregnant woman's card is filled in, which indicates the expected date of delivery and the exit on maternity leave.
Your midwife will assess your risk of venous thrombosis and/or gestational diabetes. For women at risk of gestational diabetes, the time of the glucose tolerance test is agreed. For women at risk of venous thrombosis, the midwife will teach the technique of subcutaneous injections, and the doctor will write an electronic prescription for low molecular weight heparin.
The midwife will discuss with you if you need a flu vaccine. From October to March, flu season in Estonia. In the case of influenza, pregnant women are more difficult to tolerate it, and they are more likely to develop pneumonia than non-pregnant women. With your consent, the midwife will vaccinate you against influenza and complete and issue you with a vaccination passport.
During the appointment, the midwife will ask about the nature of your work (if necessary, transfer to lighter work), lifestyle and the presence of bad habits. The midwife will talk to you about your physiological changes during pregnancy and give you advice on drinking water, taking nutritional supplements and physical activity. The midwife will give you her business card with contact details.
The midwife will talk to you about your physiological changes during pregnancy and give you advice on drinking water, taking nutritional supplements and physical activity. The midwife will give you her business card with contact details.
If your gynecologist has identified your baby at risk of spinal hernia or heart disease during the OSCAR test, the gynecologist will perform a second ultrasound to rule out suspected pathologies. In the case of twins with the same placenta, an ultrasound is performed to assess for the presence of a blood transfusion syndrome between the twins.
If you have had a preterm delivery or have been diagnosed with cervical insufficiency in previous pregnancies, you will have a vaginal examination to assess the length of your cervix and your risk of preterm delivery. If you are at increased risk of preterm birth, you will be discussed with the need for progesterone prophylaxis or cervical support sutures.
Rh-negative pregnant women whose father is Rh-positive or whose child has an Rh-conflict, and the mother's blood contains antibodies to Rh, it is suggested that a blood test be performed to assess the child's Rh factor. Mothers with a Rh-positive child are drawn up an individual pregnancy monitoring plan for early detection of Rh conflict. In the presence of anti-D, anti-C and Kell system antibodies in the blood, it is important to check for a possible increase in antibodies once a month.
During your appointment, the midwife will test your urine and take a blood sample to evaluate your hemoglobin. At the appointment, your body weight and blood pressure are measured.
If your OSCAR test result indicates an increased risk of preeclampsia, your midwife will also take a blood test to determine placental growth factor, which can be used to reassess the risk of preeclampsia.
During the visit, the midwife will ask about your baby's movements.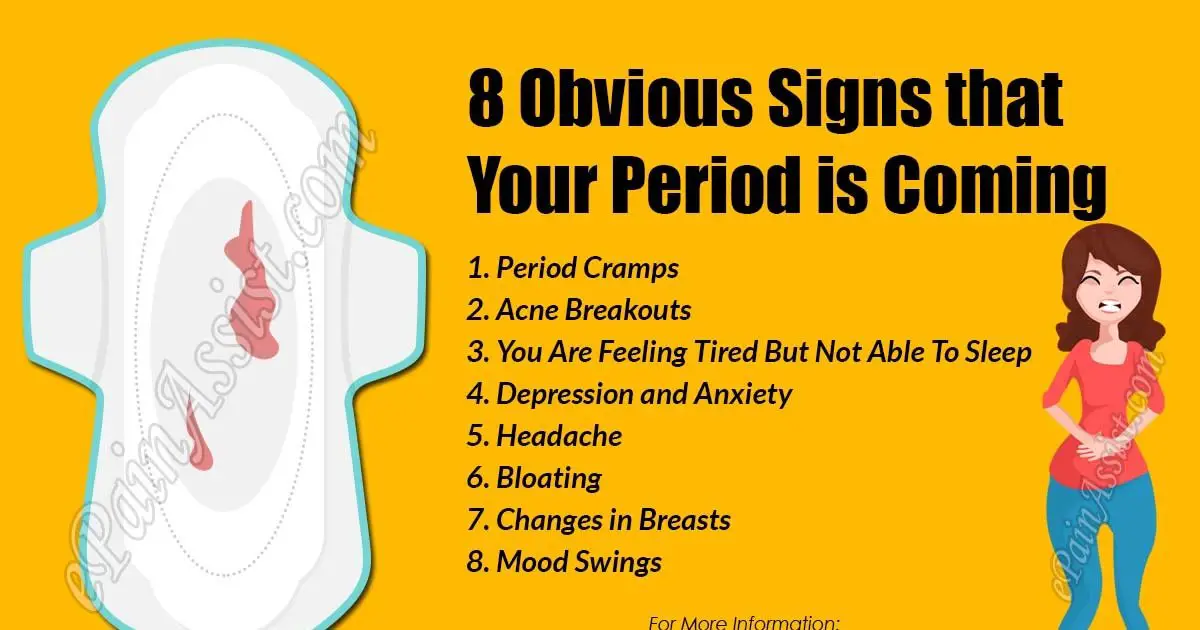 If you still do not feel the movements of the child and are worried about this, you can rent/purchase a fetal doppler from us. Your midwife will teach you how to use the fetal Doppler and find your baby's heart sounds with it. Kätlin will tell you about family schools at different maternity hospitals and the need for physical activity during pregnancy.
If you still do not feel the movements of the child and are worried about this, you can rent/purchase a fetal doppler from us. Your midwife will teach you how to use the fetal Doppler and find your baby's heart sounds with it. Kätlin will tell you about family schools at different maternity hospitals and the need for physical activity during pregnancy.
Depending on the level of hemoglobin in the blood, the midwife will assess the need for prophylactic iron replacement therapy.
The gynecologist and nurse will perform an ultrasound screening for fetal malformations in the second trimester, during which the development of your child's organ systems is assessed in detail. Particular attention is paid to the assessment of the structures of the child's brain and heart. For pregnant women with an increased risk of congenital heart defects of the child, in addition to anatomical screening, echocardiography of the child's heart is performed. If during the ultrasound there is a suspicion of a malformation of the fetal brain, in addition to anatomical screening, vaginal neurosonography of the child's brain is performed.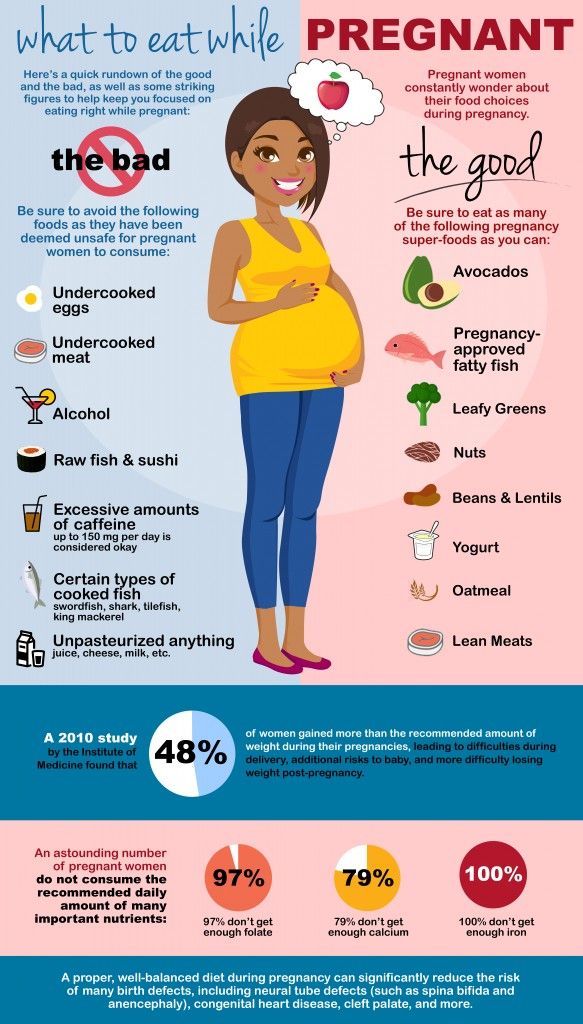
If you have an increased risk of preeclampsia on the OSCAR test, a preeclampsia risk reassessment is done to assess the effectiveness of low-dose aspirin prophylaxis and to develop a pregnancy management plan.
If indicated, the gynecologist will offer you a vaginal ultrasound to measure the length of the cervix and assess the risk of preterm birth. If you have a short cervix and an increased risk of preterm labor, your gynecologist will discuss with you the need for progesterone prophylaxis.
If you are at high risk for gestational diabetes, or if you have excessive weight gain or sugar in your urine during pregnancy, your midwife will perform your glucose stress test to rule out diabetes during pregnancy. To do this, you need to come to the Fetal Ultrasound Center in the morning and on an empty stomach. The midwife will first take a blood sample from you and ask you to drink a glucose solution, then the blood test is repeated after 1 hour and after 2 hours. If you suspect gestational diabetes as a result of a glucose tolerance test, your midwife will refer you to a diabetes nurse.
If you suspect gestational diabetes as a result of a glucose tolerance test, your midwife will refer you to a diabetes nurse.
During your appointment, the midwife will test your urine and take a blood test for the second half of your pregnancy. If you are Rh negative and the baby's father is positive, and we do not know what Rh factor your child has, then it is necessary to repeat the assessment of antibodies to Rh factor in your venous blood. If you don't have Rh antigens in your blood, your midwife will discuss with you the need for immunization to prevent Rh conflict in future pregnancies.
Pregnant women are very difficult to tolerate inflammation of the renal pelvis. Therefore, if you are at risk for urinary tract infection (chronic inflammation of the renal pelvis, recurrent white blood cells in the urine), you should take your morning urine with you so that the midwife can send it to the laboratory for pathogen testing.
Your body weight and blood pressure will be measured during the appointment. During the visit, Kätlin will ask about the nature of your child's movements and the presence of edema. The midwife will agree with you when you go on maternity leave. The midwife will teach you how to recognize the symptoms of preeclampsia. We will discuss with you the need to prepare for childbirth. If necessary, you will be consulted about ailments in the second half of pregnancy (heartburn, leg cramps, back pain, constipation).
The midwife will discuss with you the need for whooping cough vaccination. Whooping cough is an acute respiratory illness characterized by coughing fits that last for weeks or even months. Whooping cough is especially dangerous for infants, with most deaths associated with the disease in infants under three months of age. Whooping cough is one of the causes of sudden infant death syndrome. Studies have shown that the greatest transfer of anti-pertussis antibodies to the fetus through the placenta occurs in the last four weeks of pregnancy.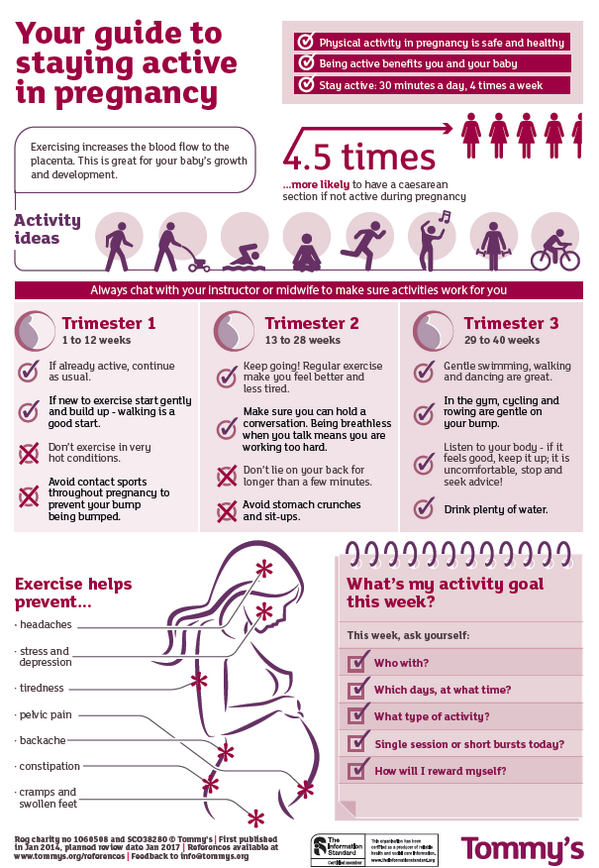 Therefore, in the third trimester of pregnancy, it is recommended to make a vaccine against diphtheria, tetanus and whooping cough. With your consent, Kätlin will vaccinate you against whooping cough and complete and issue you with a vaccination passport.
Therefore, in the third trimester of pregnancy, it is recommended to make a vaccine against diphtheria, tetanus and whooping cough. With your consent, Kätlin will vaccinate you against whooping cough and complete and issue you with a vaccination passport.
If you can't wait to see your baby, 28 weeks of pregnancy is the best time to have your 3D/4D ultrasound. At this stage of pregnancy, the child can already open his eyes, and his face already looks like the face of a newborn. At this stage of pregnancy, it is most likely that there will be enough amniotic fluid between the baby's face and the wall of the uterus. This will allow you to make a three-dimensional image of the child's face on ultrasound. It is recommended to drink plenty of fluids for three days before the ultrasound and for half an hour before the ultrasound to eat food / drink liquids with a high energy value, this will increase the likelihood that during the ultrasound your child will be awake and you will be able to see his face in the form of a moving 4-dimensional picture.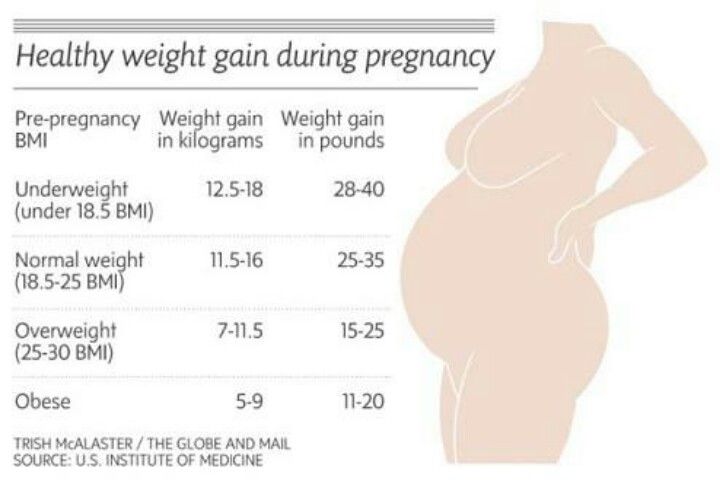
During your appointment, the midwife will test your urine and take a blood sample to evaluate your hemoglobin. If your hemoglobin level is low, your midwife will advise you on an iron-rich diet or if anemia occurs during pregnancy, prescribe iron replacement therapy.
Your body weight and blood pressure will be measured during the appointment. During the visit, the midwife will ask about the nature of your baby's movements, the presence of edema, and will do a fetal heart cardiotocography (CTG) to assess the condition of your baby and the tone of the uterus.
The midwife will advise you on the results of the CTG, discuss with you the need to prepare for childbirth, recommend getting to know the maternity ward where you want to give birth. If you wish, Kätlin will give you recommendations for finding an individual birth midwife, help you draw up a written birth plan. If necessary, you will be consulted about ailments in the second half of pregnancy.
Your midwife will reassess your risk of venous thrombosis. For women at risk of venous thrombosis, the midwife will teach the technique of subcutaneous injections, and the doctor will write an electronic prescription for low molecular weight heparin.
After the midwife's appointment, the gynecologist and nurse will perform an ultrasound to assess your baby's growth and condition. This ultrasound makes it possible to detect babies who have not reached their growth potential in utero and need more frequent monitoring and, if necessary, earlier induction of labor. This ultrasound is important primarily for those women who are at risk of having a child growth retardation.
If you have been diagnosed with growth retardation and need to be called into preterm labor, your gynecologist will perform an ultrasound scan to assess the maturity of the fetus's lungs using the QuantusFLM program. If your child's lungs are not yet mature and contain too little surfactant (a surfactant that helps keep the alveoli open), your child's lungs will be primed with betamethasone injections that will be given to you intramuscularly. When the baby's lungs have reached maturity, you will be sent to the maternity hospital to induce labor.
When the baby's lungs have reached maturity, you will be sent to the maternity hospital to induce labor.
If you are in danger of preterm labor, if your midwife's CTG reveals irregular uterine contractions, your gynecologist will perform a vaginal examination with the PartoSure test to distinguish between false contractions and actual labor. When labor begins, you will be sent to the hospital.
The thirty-second week ultrasound can also assess the risk of late preeclampsia. If there is a high risk of pre-eclampsia, the gynecologist will create an individual monitoring plan for you and your child in order to detect pre-eclampsia in a timely manner. When high blood pressure occurs, the diagnosis is clarified and high blood pressure treatment begins in a timely manner, with more frequent monitoring of you and your child. You will be taught how to monitor your blood pressure at home and how to recognize the symptoms of preeclampsia in a timely manner.
During your appointment, the midwife will test your urine and take a blood sample to evaluate your hemoglobin. At the appointment, your body weight and blood pressure are measured. During the visit, the midwife will take an interest in the nature of the movements of your child, the presence of edema and will do a CTG to assess the condition of your child and the tone of the uterus.
At the appointment, your body weight and blood pressure are measured. During the visit, the midwife will take an interest in the nature of the movements of your child, the presence of edema and will do a CTG to assess the condition of your child and the tone of the uterus.
Beta-hemolytic streptococcus (BHS) may be present in the genital tract of an expectant mother. After delivery, this microbe can cause inflammation of the uterus or meningitis or sepsis in the newborn. Women in labor who are carriers of BGS, at the beginning of labor, can be given prophylactic antibiotic treatment in the maternity hospital, which will prevent the occurrence of the complications described above. The need for testing for BGS before delivery can be discussed with the midwife.
The midwife will teach you how to recognize the onset of labor and how to behave at home if the amniotic fluid breaks prematurely. The midwife will also give advice on when to go to the maternity hospital and what to bring with you to the hospital.
After the midwife's appointment, the gynecologist and nurse will perform an ultrasound to assess your baby's height and position. This ultrasound makes it possible to detect children who have not reached their growth potential in utero and who are in the womb in a breech presentation. In the case of a breech presentation, the mother is offered an external obstetric rotation of the fetus, which is carried out in the hospital that the woman has chosen for childbirth. In half of the cases, it is possible to turn the child head presentation, which allows the mother to give birth to a child on her own. With your consent, the gynecologist will take an analysis for BGS from the surface between the labia.
If premature leakage of amniotic fluid is suspected, the gynecologist performs the Actim PROM test to assess the presence of amniotic fluid. In case of leakage of amniotic fluid, you will be sent to the maternity hospital.
At 36 weeks' gestation, all women are offered a risk assessment for late preeclampsia. Your gynecologist will make a preliminary birth plan for you. If you need a planned caesarean section, the gynecologist will give you a referral to the maternity hospital.
Your gynecologist will make a preliminary birth plan for you. If you need a planned caesarean section, the gynecologist will give you a referral to the maternity hospital.
During your appointment, the midwife will test your urine and take a blood sample to evaluate your hemoglobin. At the appointment, your body weight and blood pressure are measured. During the visit, the midwife will take an interest in the nature of the movements of your child, the presence of edema and will do a CTG to assess the condition of your child and the tone of the uterus.
The midwife will advise you about the postpartum adjustment of the baby, breastfeeding and newborn care, and will discuss with you the follow-up monitoring of the newborn by the family doctor or pediatrician.
During your appointment, the midwife will test your urine and take a blood sample to evaluate your hemoglobin.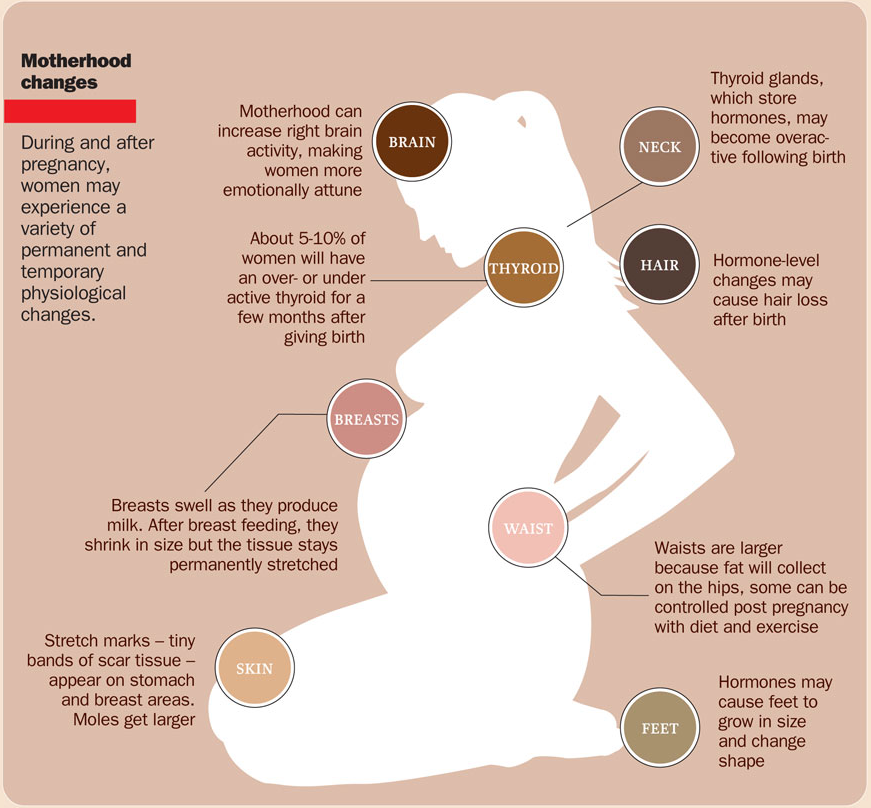 During the appointment, your body weight and blood pressure will be measured. During the visit, the midwife will take an interest in the nature of the movements of your child, the presence of edema and will do a CTG to assess the condition of your child and the tone of the uterus. The midwife will advise you about the postpartum period and recommend when to visit your gynecologist for a postpartum checkup. Katlin will help you if you have problems with breastfeeding, and you can always come to her appointment.
During the appointment, your body weight and blood pressure will be measured. During the visit, the midwife will take an interest in the nature of the movements of your child, the presence of edema and will do a CTG to assess the condition of your child and the tone of the uterus. The midwife will advise you about the postpartum period and recommend when to visit your gynecologist for a postpartum checkup. Katlin will help you if you have problems with breastfeeding, and you can always come to her appointment.
During your appointment, the midwife will test your urine and take a blood sample to evaluate your hemoglobin. During the appointment, your body weight and blood pressure will be measured. During the visit, the midwife will take an interest in the nature of the movements of your child, the presence of edema and will do a CTG to assess the condition of your child and the tone of the uterus.
After the midwife's appointment, the gynecologist will evaluate the length and maturity of the cervix, as well as the possibility of spontaneous delivery, using a vaginal ultrasound and probing.
If the cervix is immature, the gynecologist will begin, with your consent, the preparation of the cervix using progesterone vaginal gel.
If there are abnormalities in the course of pregnancy, for example, tests performed during pregnancy are not in order, a complicated pregnancy, or you have some kind of internal disease, the interval for monitoring the pregnancy and the study plan will depend on the specific case of the disease. Monitoring of dichorionic (with two placentas) twins will be carried out by a gynecologist and an obstetrician at 4-week intervals, and monitoring of monochorionic twins at 2-week intervals. Monitoring of stunted fetuses should be done at two- or one-week intervals, depending on the condition of the child.
In cooperation with the best specialists in their field, if necessary, you will be referred to a Stage III hospital for further investigations and treatment.
For women registered with the Fetal Ultrasound Center, all ultrasound examinations after registration for pregnancy are 10% cheaper .